The AAMC (Association of American Medical Colleges) is sounding the alarm on the cumulative impact of federal actions proposed by Congress and the administration, warning that together, they represent an existential threat to the nation’s medical schools, academic health systems, and biomedical research institutions.
Already in 2025, the termination of more than 1,100 National Institutes of Health (NIH) grants has imperiled cutting-edge research at dozens of academic centers, according to a June 2025 report released by the AAMC. These include the reported termination of at least 160 clinical trials designed to study areas such as HIV/AIDS, mental or behavioral health conditions, cancer, substance use, and chronic diseases.
“For decades, NIH-funded research has driven groundbreaking medical discoveries and cemented America's position as the global leader in medical diagnosis, technology, and cutting-edge treatments,” says David J. Skorton, MD, AAMC president and CEO. “The impact of funding cuts does not stop at university walls; it reverberates through the lives of millions of Americans facing cancer, diabetes, Alzheimer’s, and many other illnesses. When we undermine our research institutions, we sacrifice the health and well-being of our nation.”
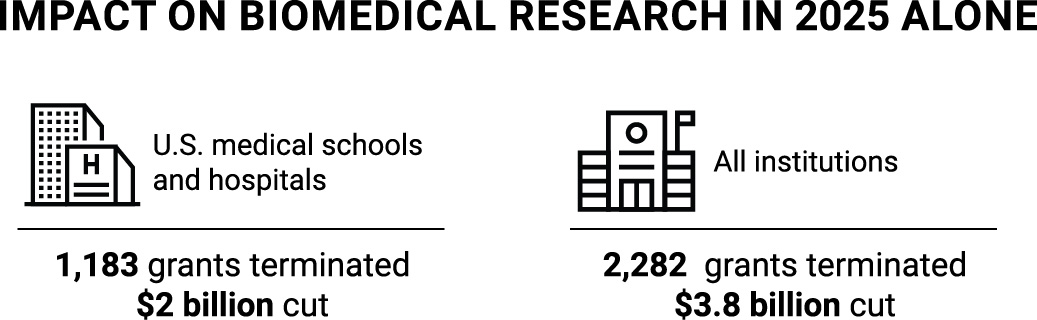
As devastating as the cuts to NIH-funded grants in 2025 have been, they represent just one of many threats to academic medicine and the health of millions of patients who receive care at our nation’s academic health systems.
- Medicaid: Proposed cuts to states that fund Medicaid through provider taxes and that expanded their coverage under the Affordable Care Act, as well as a proposed work requirement for adults 18-64 receiving Medicaid, will result in nearly 11 million people losing access to health insurance by 2034, according to estimates from the Congressional Budget Office. Without regular access to care, many of those patients will end up in the emergency department, often when they are sicker and need more complex care. AAMC member academic health systems represent 5% of all hospitals but provide 32% of all uncompensated care.
- Student loans: The proposed elimination of federal student aid programs like Grad PLUS loans and changes to eligibility requirements for Public Service Loan Forgiveness would impact nearly half of all medical students, with devastating consequences. “Eliminating or restricting these critical programs would undermine the future physician workforce and ultimately make it harder for patients in communities nationwide to get the care they need,” Skorton said.
- NIH: In February, the NIH announced that it would limit indirect costs for research grants to 15%, which would have cut $6.5 billion from the research enterprise. Indirect costs — or facilities and administrative (F&A) fees — support research operations, including data processing, utilities, state-of-the-art laboratories, patient safety personnel, and more. Academic institutions are reimbursed by the federal government for part of these expenses at negotiated rates. In fact, without these additional funds, some research would not continue. Clinical trial patients would lose access to what, for some, might be their last hope for treatment. The loss of basic science research would slow scientific progress. The AAMC filed a lawsuit that halted the proposed cuts to F&A costs in February, but the administration has signaled that it intends to pursue the measure in its FY 2026 budget. The administration has proposed cuts to NIH of $18 billion for FY 2026, which begins in October.
- Disproportionate share hospital (DSH) payments: Safety-net hospitals and the patients they serve were dealt a crushing blow in April 2025, when the Supreme Court ruled that the hospitals were not entitled to reimbursement for the care of some patients. The Centers for Medicare & Medicaid Services (CMS) provides DSH payments to hospitals that care for a disproportionate share of low-income patients; the ruling could jeopardize the care that hospitals can provide to those patients.
- Lower Medicare reimbursements: Academic health systems serve disproportionately higher numbers of Medicare patients, whose care is often more complex than that of younger and healthier patients. But reimbursement rates for Medicare patients remain stubbornly lower than rates for privately insured patients, putting an additional burden on hospitals. In fact, Medicare covered less than 84% of average hospital costs in FY 2020. The 2025 Medicare Physician Fee Schedule finalized by CMS included a 2.83% cut across the board. That follows a 1.69% Medicare pay cut in 2024 and a 2% cut in 2023. In total, Medicare physician payment has declined by 29%, adjusted for inflation, from 2001 to 2024.
- Hospital outpatient departments (HOPDs): Academic health systems provide more than just inpatient care. They also provide outpatient, clinic-based care that increases access to crucial services. Several proposals in Congress would reduce payments at these clinics, lowering them to the amount paid at physician’s offices – so called site-neutral payments – despite the higher costs associated with operating a comprehensive health system. These proposals could cost providers as much as $167 billion over 10 years.
- 340B: Under the 340B drug pricing program, passed by Congress in 1992, drug companies are required to provide discounts to hospitals that treat a disproportionate number of low-income patients. Recently, drug makers have attempted to transform 340B into a rebate model. While these efforts are opposed by HRSA and hospital 340B providers, drug makers have challenged that position through several lawsuits . According to the nonprofit advocacy group 340 Health, 340B hospitals provide 77% of Medicaid hospital care and 67% of all uncompensated care. The AAMC continues to urge policymakers to oppose policies that would reduce reimbursement for 340B-acquired drugs, noting that they would erode the savings available to safety-net providers and harm the patients and communities they serve.
“The NIH cuts have already caused immense devastation — and now, these additional actions compound that harm on an even greater scale,” says AAMC Chief Health Care Officer Jonathan B. Jaffery, MD, MS, MMM, FACP. “We’re talking hundreds of millions of dollars in cuts that would lead to the discontinuation of some clinical services and require deep layoffs — thousands or even tens of thousands of health care workers could be impacted.”

Threats to academic medicine put America’s health at risk
Academic medicine plays a unique role in the U.S. health care system. Not only do academic health systems house the most advanced biomedical research facilities, but they also are comprised of medical schools and teaching hospitals that educate the next generation of physicians and treat some of the sickest and most complex medical cases.
“Collectively, if all of the proposed actions are approved, the impact on academic medicine will be enormous,” says AAMC Chief Public Policy Officer Danielle Turnipseed, JD. “Academic health systems can only absorb so much without significant harm to biomedical research, medical education, and patient care.”
Here’s what’s at stake:
Academic medicine is a global leader in complex patient care
- In early May, surgeons from two academic medical centers — the University of California, Los Angeles (UCLA), and the University of Southern California (USC) — performed the first human bladder transplant in a 41-year-old man who had lost most of his bladder during surgery to remove a cancerous tumor. The historic surgery was the result of years of research by surgeons at the UCLA David Geffen School of Medicine and the USC Keck School of Medicine. They plan to perform transplants on additional patients as part of a clinical trial to validate the procedure, which could ultimately improve the lives of thousands of patients.
- In 2023, an Arkansas man became the world’s first recipient of a total-eye and partial-face transplant, after the former lineman hit an exposed wire while working on utility repairs. The surgery, which required the expertise of more than 140 medical professionals, was made possible by the skilled surgeons at NYU Langone, an academic health system in New York City.
- At West Virginia University School of Medicine (WVU), researchers are exploring treatments to prevent diabetic retinopathy, a complication of diabetes that can cause blindness.
- The NIH funded the development of the first artificial heart valve, including the first successful replacement at the NIH Clinical Center in 1960. Today, more than 100,000 heart valve replacements are performed each year in the United States.
- According to a study published in JAMA, patients treated at major teaching hospitals have up to 20% higher odds of survival (PDF), compared to those treated at nonteaching hospitals.
Academic health systems conduct the majority of all NIH-funded research
NIH-funded research at academic health systems is the reason why the United States has been a global leader in biomedical research and scientific discovery. In FY 2025, approximately $37 billion in NIH-funded research supported more than 300,000 researchers at over 2,500 institutions in all 50 states and the District of Columbia.

- At the University of Kentucky College of Medicine, researchers are engaged in 708 active clinical trials exploring treatments for cardiovascular disease, cancer, diabetes and obesity, and more.
- NIH funding at academic health systems has also played a pivotal role in new drug development, with one study noting that “NIH funding contributed to research associated with every new drug approved from 2010-2019,” totaling more than 350 products.
Academic health systems provide essential services unavailable elsewhere
-
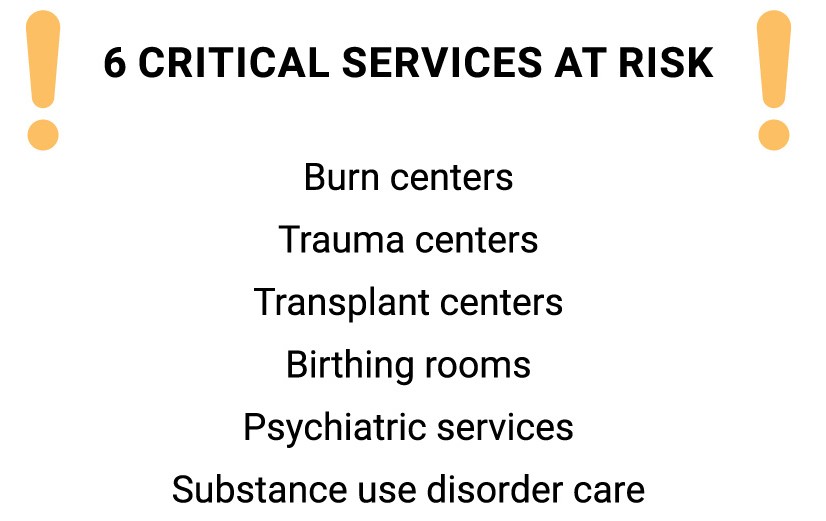
- Academic health systems house 100% of all National Cancer Institutes registered cancer treatment centers, 59% of all Level I trauma centers, and 64% of all pediatric intensive care unit beds.
Academic health systems train the next generation of physicians
- Academic health systems train the future physician workforce. Each year, AAMC member medical schools and teaching hospitals train approximately 77,000 residents nationwide, making them the primary producers of both primary care and specialty physicians. Of these residents, Medicare offsets a portion of the costs for approximately 57,000 trainees. AAMC-member teaching hospitals fully cover the costs of training the remaining 20,000 residents— an estimated $18.7 billion annually.
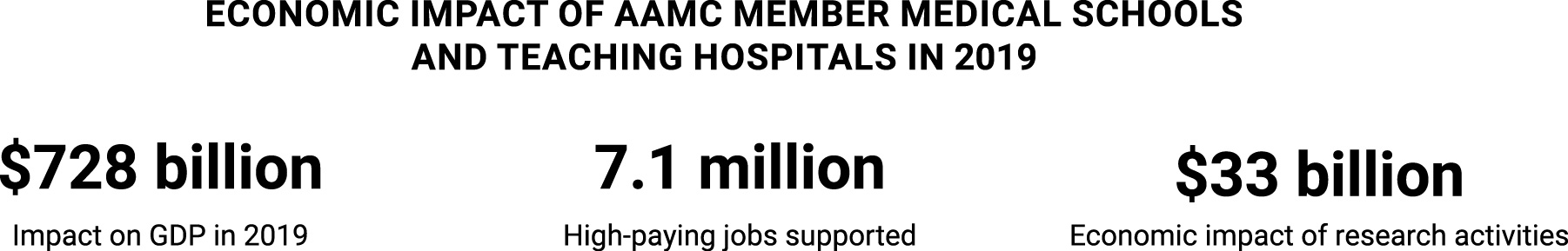
Academic health systems are economic engines for their communities
- An AAMC study on the economic impact of AAMC member medical schools and academic health systems highlights their significant contributions to the nation’s economy. According to the study, academic health systems added more than $728 billion to the U.S. economy in 2019 and supported more than 7.1 million high-paying jobs. Medical research investments and activities at medical schools and academic health systems alone play a significant role in the economic health of communities across the country. The report found that these activities added $33 billion to the nation’s economy, including 348,000 related jobs. Collectively, every dollar spent by AAMC-member institutions contributes $1.62 to the U.S. economy.
Proposed federal actions on multiple fronts not only jeopardize scientific discovery and individual Medicaid patients who might lose health insurance. They jeopardize the entire academic medicine ecosystem — the trauma and burn centers that care for people who suffer horrific accidents; the cancer centers that offer patients hope through new and innovative treatments; the emergency services that treat everyone who walks in the door, regardless of their ability to pay; the medical students and residents whose education and training are critical to treating future patients; the future heart disease, diabetes, and cancer patients who will no longer benefit from the scientific discoveries that can’t happen without research support; and the ability of academic medicine to continue to provide world-class treatment to all patients.
“For generations, bipartisan leaders have recognized that America’s strength and future rely on the groundbreaking research performed at our nation’s biomedical research facilities, the complex and highly sophisticated care provided at academic health systems that is the envy of the world, and the ability of our medical schools and teaching hospitals to train the next generation of physicians," said Skorton. “For the sake of medical advancement, economic prosperity, and the health of every citizen, we need policymakers to work with us, not against us. The stakes could not be higher — lives truly hang in the balance.”
For more information or to request an interview with an AAMC subject matter expert, please contact press@aamc.org.
