Although 1 in 5 adults in the United States had a mental illness in 2020, over half of those affected did not receive treatment1 because of barriers to accessing care.2 One significant barrier is the shortage of psychiatrists across the country.3 While research and policy tend to focus on psychiatrists and psychologists,4 other mental health professionals (e.g., social workers, counselors, and marriage and family therapists) represent a large share of the behavioral health workforce and provide a significant amount of behavioral health care.5 The training and expertise of each of these groups of mental health professionals also varies, which is important for health care providers and consumers to understand.
This snapshot summarizes the qualifications, educational requirements, and distribution of some of the main groups of independently licensed mental health providers across the country. While training and recruiting more doctors specializing in psychiatry is necessary, physicians will not alone be able to meet the needs of the more than 57 million people in the United States living with mental illness.6
Different Positions
The behavioral health workforce typically includes psychiatrists, psychologists, social workers, counselors, marriage and family therapists, and others — depending on the health care model and organization. Table 1 outlines the number of providers in each profession in the United States and their duration of education and training. These providers may specialize and receive their licenses or certificates from professional and state boards.7 The length of education and training remains the longest for psychiatrists (eight to 10 years), followed by psychologists (five to 10 years). Psychiatrists, unlike social workers, counselors, or marriage and family therapists, may prescribe medications to patients.8 Currently, five states allow psychologists to obtain certification to prescribe medication.9 Psychiatrists also typically see patients for shorter visits, and 53% no longer deliver psychotherapy.10,11,12 Although increasing the number of psychiatrists and psychologists is important, collaboration and promotion of task shifting13 may help better distribute providers to match need.
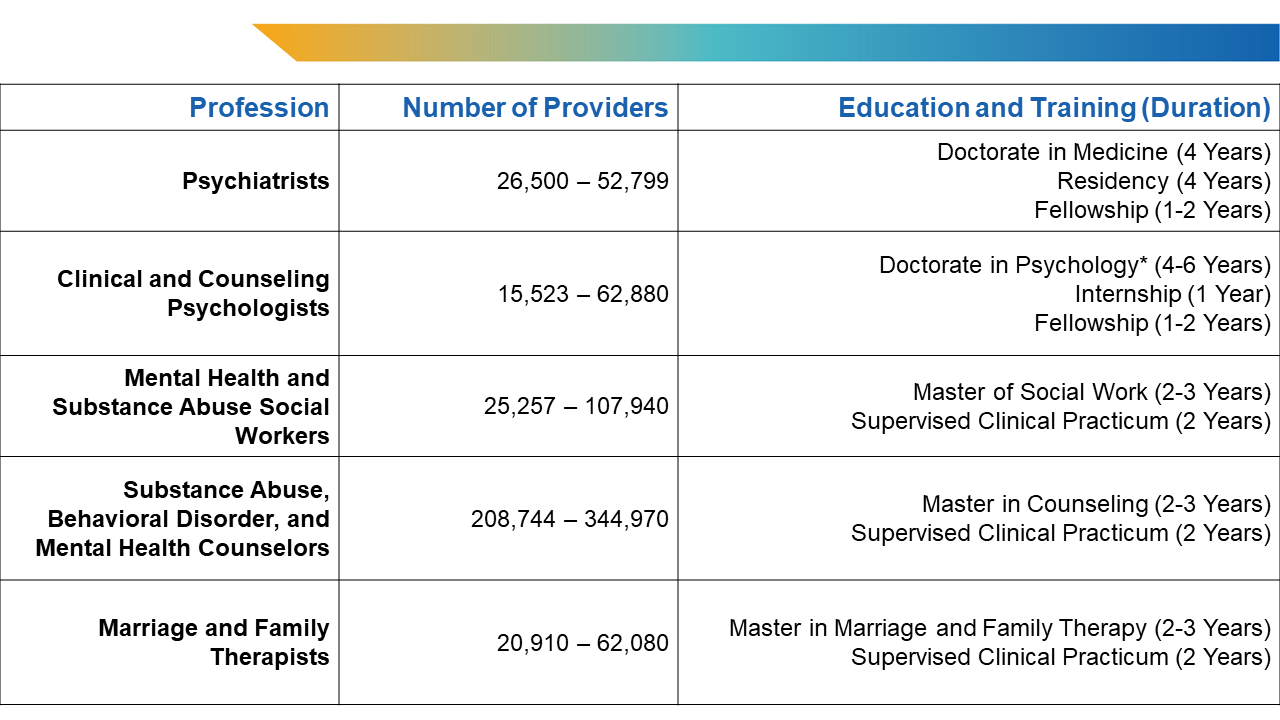
Table 1: Prevalence, Education, and Training of Mental Health Professionals in the United States.
*Certain state requirements allow individuals to practice after receiving their licensure and completing a master in psychology. Providers with a doctorate of philosophy in clinical or counseling disciplines are also qualified.
Sources: U.S. Bureau of Labor Statistics. May 2022 National Occupational Employment and Wage Estimates; American Board of Medical Specialties. Board Certification Report 2021-2022; United States Census Bureau. 2021 American Community Survey Data.
Notably, Table 1 does not reflect all potential degrees and titles. For example, there are entry-level and assistant positions for social workers and counselors with an undergraduate education, but only behavioral health graduate degrees are displayed in Table 1. Despite opportunities for mental health certification and training, only 6.5% of nurse practitioners (NPs)14 and 2.0% of physician associates (PAs)15 reported a primary certification or specialized training in psychiatry or mental health. Primary care providers (PCPs) also frequently represent a first entry point for patients into the mental health care system. Adults with a major depressive episode were more likely to talk about their feelings with a general practitioner or family doctor (50.4%) than with a psychiatrist (39.4%) in 2021.2,6 These numbers underscore the need for increased behavioral health access and integration in primary care settings. While PCPs may receive behavioral health training during residency,16 few choose to complete additional specializations17 — only 1,833 physicians are certified in addiction medicine.18 Finally, nonlicensed professionals such as community health workers and peer networks also extend important types of support.19,20
Overview of Shortages
Nationally, projections have revealed an estimated shortage of between 14,280 and 31,081 psychiatrists by 2024.21 Over half (51%) of counties in the United States lack practicing psychiatrists.22 The number of psychiatry residency applicants has also declined over the past two years.23 Alarmingly, factors such as burnout,24 retirement,25 and lower rates of reimbursement, which dissuades providers from accepting insurance,26 may lead to a 20% decrease in the number of adult psychiatrists by 2030.27
However, substantial growth across other behavioral health disciplines is expected, including a 114% increase in the supply of social workers and a 37% increase in the supply of marriage and family therapists.27 Recent proposals also suggest that expanding the roles of PAs and psychiatric advanced practice nurses (APRNs) may reduce behavioral health workforce shortages, especially in rural communities that lack specialized clinicians.2,28 Many PAs and APRNs have prescriptive authority, but that depends on state scope-of-practice laws.29,30
