More students. More professors. More deans. The numbers document the many gains that women have made in U.S. medical schools over the past two decades.
But the advances have been incremental, and some data demonstrate the challenges that continue: Pay and faculty rank still lag behind what they are for men, and the work environment is frequently hostile.
Those are among the findings in a report released this week by the Association of American Medical Colleges (AAMC), The State of Women in Academic Medicine: Progressing Toward Equity, 2023-2024.
“The data in this report illustrate the significant increase in women’s representation across key career milestones,” the report states. But the data also highlight “the institutional structures and climate issues that require further attention if we are to continue progress toward gender equity and organizational excellence.”
AAMC has published a national snapshot of women learners, faculty, and administrative leaders in academic medicine since 1983. Below are highlights from this year’s report and observations about some of the findings.
Women account for an increasing majority of students who apply to and graduate from medical school.
Here is how the percentage of women in those groups has changed over time, by school year:
- Applicants
- 2000-01 — 47%
- 2023-24 — 57%
- Graduates
- 2000-01 — 43%
- 2022-23 — 52%
What’s more, according to previously released data from the AAMC, in 2023-24 women accounted for 54.6% of medical school students, after having become a majority for the first time in 2019-20.
The increasing presence of women in medical school is a fundamental reason for their growing presence in teaching and leadership, notes Diana Lautenberger, director of gender equity initiatives at the AAMC.
“If the majority of medical school students and graduates are women, it bears out later along the [career] pathway, through faculty and leadership, that there will be more women,” she says.
More women are on the faculties of medical schools
Here is how the percentage of faculty that are women has changed over the past decade:
- 2013 — 38%
- 2023 — 45%
More specifically, for 2023-24 alone, women made up:
- 45% of full-time faculty
- 29% of full-time professors
- The majority (52%) of faculty in one area: those with PhDs in clinical science
- Women make up a minority of faculty with MDs and MD-PhDs in clinical science and basic science.
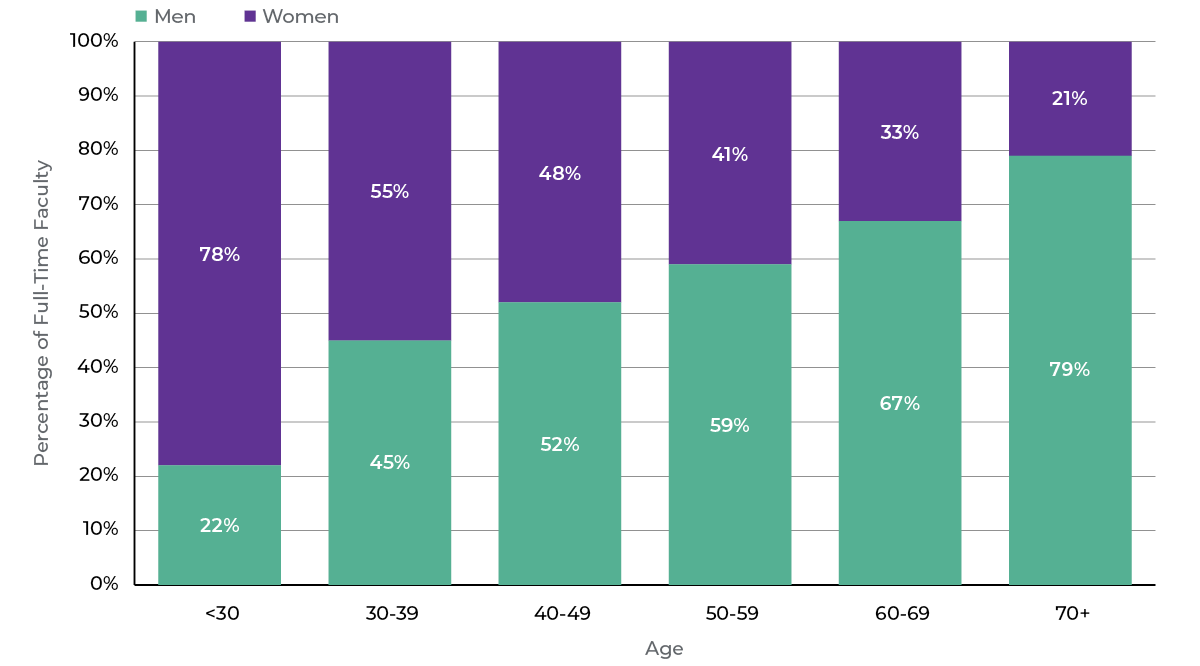
Women account for most of the younger faculty, while men account for most of the older faculty
This reflects the recent growth of more women graduates gradually moving into teaching positions. Here are the percentages of women faculty by age groups:
More women are in leadership positions in medical schools
But the rate of growth lags behind their expansion as students and physicians. Here is how the percentage of women in several top positions has changed over the years:
- Division and section chiefs
- 2013 — 24%
- 2023 — 34%
- Center and institute directors
- 2018 — 30%
- 2023 — 32%
- Department chairs
- 2013 — 15%
- 2023 — 25%
- Deans
- 2013 — 16%
- 2023 — 27%
The report also collected, for the first time, data on the gender of health system CEOs. In 2023, 25% were women.
“We’re making steady progress,” Lautenberger says. But she notes that women’s representation in leadership positions has not kept pace with the rising proportion of women medical students and physicians over the past several decades. In the 1990s, she points out, about 40% of medical students were women, and “we should see similar proportions of women in top leadership positions by now.
“That tells us that there are other systemic issues at the institution level that we really need to be addressing if we hope to make progress,” Lautenberger adds.
Pay equity is improving, but the gaps with men remain
Women in medicine continue to be paid less than men in the same positions, although the disparity is shrinking. Here are examples of the median compensation on the dollar for women faculty, compared with men, based on department type, degree, and rank in 2022:
- Clinical MD, associate professor — 78¢
- Clinical MD, full professor — 83¢
- Clinical PhD, full professor — 94¢
- Basic science PhD, full professor — 98¢
- Basic science PhD, associate professor — 99¢
The gender pay gap begins at the start of medical careers and tends to expand over time due to professional advancement and compensation disparities, says Amy S. Gottlieb, MD, chair of the AAMC’s Group on Women in Medicine and Science Steering Committee.
“There are multiple inflection points in women’s career trajectories where academic medicine’s traditional way of compensating faculty disadvantages them,” says Gottlieb, author of Closing the Gender Pay Gap in Medicine: A Roadmap for Healthcare Organizations and the Women Physicians Who Work for Them.
For example, “research consistently shows that women earn less than their male counterparts right out of training. In setting salaries, there is often a considerable difference between the dollar amounts at the low and high ends of the benchmark ranges, allowing organizations a wide berth in determining compensation.”
Gottlieb urges academic medical leaders to “explore how their pay practices are inadvertently perpetuating salary inequities” through embedded processes and structures. “My experience is that most people believe in equal pay for equal work, but it’s how to achieve this goal that can overwhelm institutions and leaders.”
Gender harassment is common
Nearly one in three women (31%) report experiencing gender harassment in the medical school workplace, “highlighting the urgent need for cultural and systemic changes to create a safer and more inclusive environment,” the report says. Here are rates of reported harassment:
- Men – 12%
- Women — 31%
- Heterosexual men — 12%
- Heterosexual women — 30%
- LGB-plus men — 18%
- LGB-plus women — 44%
Lautenberger says gender harassment is one of several factors — including low pay and other types of harassment — that push many women out of academic medicine, which in turn contributes to the gaps in faculty leadership and pay further down the career path.
“What I hear is that women are being pushed out because of the climate and the culture,” Lautenberger says. “If there are pay inequities, if you are isolated in your department, if you face microaggressions and bias every day, if you’re being sexually harassed, if your abilities are being doubted, if you are not being promoted — a lot of people say, ‘I can’t survive in this environment. I will go into my own private practice or leave medicine altogether.’ That’s bad not just for women, but academic medicine generally.”
The report provides strategies for institutions to advance gender equity in pay and working conditions, including removing biases from systems and processes, establishing equitable policies for caregiving, and creating safe reporting mechanisms for harassment and bias.

