When Hahnemann University Hospital in Philadelphia announced it would be closing, it set in motion a chain of events that affects everyone from students and residents to program directors, faculty, and patients. Here’s what you need to know, whether you’re at Hahnemann or another academic medical institution.

On June 26, 2019, Hahnemann University Hospital, the primary teaching hospital affiliated with Drexel University College of Medicine in Philadelphia, Pennsylvania, announced that it was filing for bankruptcy and would be closing its doors in late September. Hospital administrators have since informed state regulators that they are likely to close even earlier, possibly at the end of the August.
At the time of the announcement, approximately 100 patients were being cared for at Hahnemann — and 571 residents and fellows, as well as some Drexel medical students, were in training there. All will be displaced once the hospital is shuttered.
In addition to affecting patients, the closure sent ripples through the academic medicine community, as Hahnemann residents scramble to find slots elsewhere, program directors at other institutions inquire about taking these residents, and the organizations supporting resident education — including the AAMC, the Accreditation Council for Graduate Medical Education (ACGME), the Educational Commission for Foreign Medical Graduates (ECFMG), and the Centers for Medicare and Medicaid Services (CMS) — step up to offer assistance and guidance.
Let’s talk first about the medical students at Drexel University College of Medicine. Many of them were doing their third- and fourth-year rotations at Hahnemann. What is happening on that front?
We have been advised by the dean’s office that all medical student rotations for the third and fourth years have been transferred to other clinical sites. So we know that all medical students have been removed and are in appropriate training sites right now.
That leaves the 571 residents and fellows who are training at Hahnemann. Aren’t most residencies filled during The Match®? How are these residents going to continue their training? Do they have a choice about where they go?
Our member institutions have been asked to see who might be able to take some of these residents. Here’s how it works. Let’s say that your institution’s program in internal medicine is approved by the ACGME for 30 residents, but you only have 28 residents. You can go ahead and fill those two slots right now without talking to anyone. The AAMC tracks open positions at Find a Resident, and any resident can go online and look for those open slots.
Now say that your institution has 30 positions but all 30 are taken. But as a program director, Designated Institutional Official (DIO), or other institutional official, you have enough clinical material and enough teachers that you could take a couple more residents. In that case, the program director would have to call the ACGME and get approval through an application process to temporarily increase the number of residents in their program from 30 to 32.
In the case of Hahnemann, the program directors there are also calling and looking for slots for their residents as well as looking for other clinical partners that may house their programs. So it’s an individual effort to find a slot, and that individual effort is aided by their program director as well as by the AAMC, ACGME, and ECFMG.
The closing hospital cannot direct residents to go to a particular program. Once a program is identified that will accept the resident, it is the resident’s decision about whether to go to that program or to try and find an alternative.
Residency positions are partially funded by the federal government and partially funded by the teaching hospital or another source. How do institutions who agree to take additional residents get paid?
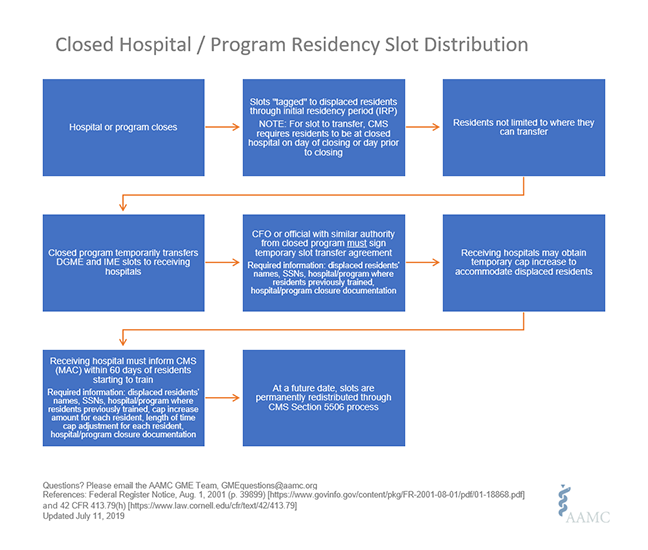
Medicare rules about what happens to graduate medical education (GME) funding when a teaching hospital closes are very complicated. The AAMC has put together a fact sheet on the basics, but I’ll try to explain it briefly here. There are two phases to consider when thinking about the funding of new residents. Phase one is the Temporary Cap Transfer. If a resident goes from Hahnemann to another teaching hospital, the resident takes one of Hahnemann’s Medicare-funded residency positions with them — after the CFO of Hahnemann signs off on the transfer — to the new hospital for the remainder of that resident’s training in the same specialty in which he or she was training at Hahnemann. The new hospital must contact their CMS Medicare Audit Contractor within 60 days and say, I have this resident. This is their demographic information, this is their name and Social Security number, and this is the document from Hahnemann saying that the hospital is closing and they’re transferring this slot with this particular resident to us.
What that means for the other teaching hospital is that it will receive two forms of funding. One is direct GME funding. That pays about 30% to 40% of the direct expense of training a resident. The second is an add-on payment to their Medicare payment, which is based on the number of Medicare patients, the capacity of the hospital, and the number of medical residents. So those two payments — the direct GME funds and the indirect medical education funds — will increase if you have appropriately applied for and gotten approval for the transfer of a resident to your program. And those payments will stay with your institution until the resident finishes the current program that they are in.
It’s the temporary transfer of funding for that slot that follows a resident so he or she can successfully complete a program. The payment from CMS is at the same rate that the receiving hospital is paid for all residents it currently is training.
If my institution accepts additional residents, will those residency slots be permanently allocated to my institution? Or will those slots disappear once those residents finish their training?
The AAMC years ago worked to ensure that the Affordable Care Act included a provision for the permanent distribution of slots when a teaching hospital closes. At some point in the future, CMS may announce a process for a permanent redistribution of the Hahnemann slots.
Any institution could submit an application for these slots. They would be distributed according to a number of criteria established by CMS. Preference is given to institutions in the same core-based statistical area in which the closed hospital is located. They will also give priority to institutions who say, for instance, “You know, Hahnemann had a really great internal medicine program. We are going to subsume the entire program and continue it at our institution,” or “We can’t take the whole program but we’re going to take some portion of it.” That would also give them priority.
So that’s the second phase of funding — the Permanent Cap Transfer — but that won’t happen for a while.
A number of Hahnemann residents are international students whose J-1 visas depend upon employment at the hospital. What will happen to them?
There are about 59 visa-holding residents who, if they don’t find a spot within 30 days of the hospital closing, will have to leave the country. We are working very closely with the ECFMG in order to help those people who have moved themselves and their families to the United States to continue with their training.
What is happening to the patients being cared for at Hahnemann? Will they be able to quickly get care at other hospitals?
The state and the city are very concerned about the safety and well-being not only of those who are employed by the hospital but also those patients who are in the hospital. The Pennsylvania Department of Health has a senior official at the hospital now who is working with staff to ensure the safety of those patients.
How about the faculty who were teaching those residents?
The faculty are also faculty at Drexel, but Drexel gets a significant amount of money from Hahnemann that supports their directorships and clinical activity. Both John Prescott, MD, AAMC’s chief academic officer, and I have been in touch with senior people at Drexel and we continue to provide support to them as they recalibrate and look at who their new clinical partners will be in the future.
In the end, it’s a complicated situation, but the AAMC is here to help. We have experts who understand the process. We can be reached at GMEquestions@aamc.org or by emailing me at jorlowski@aamc.org. We also have resources [see Related Resources] that are available to help residents, program directors, and faculty.
