Nearly 30 years ago, in an effort to address a concern that patients’ pain was undertreated, pain experts and health care organizations initiated a movement to treat pain as “the fifth vital sign.” This led doctors to control pain aggressively and use opioids liberally. And likely related, the amount of opioids sold has quadrupled since 1999, according to the Centers for Disease Control and Prevention (CDC).
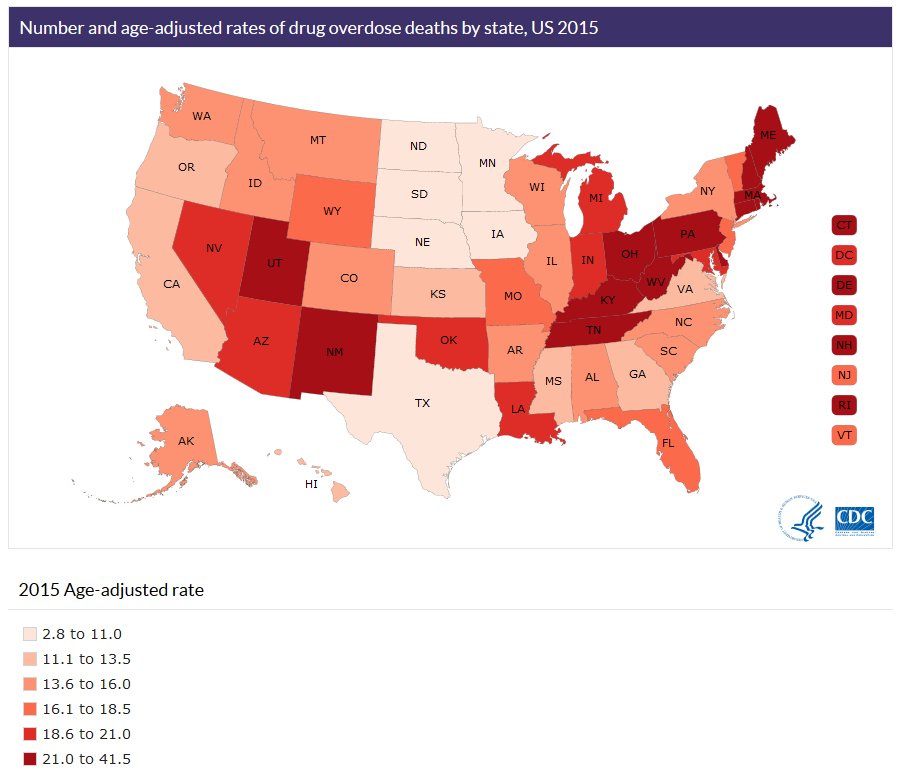
Today, we’re in the midst of what is widely considered an opioid epidemic. Prescription rates have climbed most rapidly among family practice, general practice, and internal medicine. In 2014, more than 240 million prescriptions were written for opioids—“more than enough to give every American adult their own bottle of pills,” reported the U.S. Department of Health and Human Services (HHS). In 2015, more than 22,000 people died from prescription opioid overdoses, the CDC found. Public health officials also have identified a sharp increase in heroin-related deaths. This is significant because four in five new heroin users started by misusing prescription opioids, according to HHS.
“Even with all the public scrutiny and the legislation and the policies and the media, there are still doctors out there who seem to be completely unaware of this problem and the shifting paradigm in terms of how we need to practice,” said Anna Lembke, MD, a psychiatrist and addiction specialist at Stanford University Medical Center, and author of Drug Dealer, MD: How Doctors Were Duped, Patients Got Hooked, and Why It’s So Hard to Stop. “I see this when patients come in on just astronomically high doses of opioids for chronic pain conditions—from headache to abdominal pain to lower back pain.”
Efforts to reverse these trends are complicated by the wide range of social and other factors that are contributing to the epidemic. Within the health care provider community, many experts have focused on changing prescription practices as a strategy to prevent future cases.
“Doctors [in all specialties] need to have an understanding of the process of addiction and the risks of opioid prescribing.”
Anna Lembke, MD
Stanford University Medical Center
Medical schools and physician training programs nationwide have been enhancing content on pain and addiction to reach practitioners early in their careers. “There has been a huge effort at the state, federal and local levels to better educate doctors [about opioids]. Doctors [in all specialties] need to have an understanding of the process of addiction and the risks of opioid prescribing,” said Lembke, one of three physicians presenting at an AAMC webinar on Feb. 27 about opioid addiction and public health issues.
But how can the profession reach practicing doctors, many of whom began their careers in the days when the expectation was to control pain at all costs and may not be as sensitive to the dangers of addiction? New CDC prescription guidelines and other medical board and institutional initiatives have tried to help providers weigh the benefits of opioids to control pain against other potential alternatives and the dangers of addiction.
“There is a significant effort in teaching hospitals and in other academic settings to try to move away from [older] practice patterns that were meant to provide pain control but probably inadvertently contributed to the overall epidemic," said Janis Orlowski, MD, MACP, AAMC chief health care officer. “And what you also see is an effort not only in clinical practice but also new research underway to try to better understand the problem and shift practice. I would say, good people trying to do the right thing.”
The need for continuing physician education
Medical schools and health care organizations have been developing continuing medical education programs that focus on opioids. This has always been a critical component of effective physician practice, particularly since medical knowledge is likely to evolve substantially over the course of a physician’s career. From April 5 to 7, the AAMC also will host three one-hour sessions on educating physicians about opioids that will focus on UME, GME, and CME.
Health care experts say there are numerous opportunities to stem opioid addiction through the traditional methods used to help physicians stay current with the best practices to improve patient care. The AAMC’s open-access, peer-reviewed publication MedEdPORTAL® is seeking submissions on opioids education. Potential topics include, but are not limited to, educational approaches that address alternative pain management strategies, addiction treatment options, and safe opioid prescribing. Full submission details are available at MedEdPORTAL.
Preventing the problem is a first step. Orlowski describes an approach based on a patient agreement to a contract from the physician stating, “I will continue to treat your pain but you must agree to get your opioids only from me.” The “opioid contract,” based on best practices, should also state, “You must be willing to come in and have a drug test. You must be willing to come in and have a pill count,” Orlowski said about some of the elements that might be found in such a contract.
Doctors also can consider prescribing a smaller supply of pills for a shorter period—or similarly, to fill only part of a prescription. A person can go to a pharmacist for the rest of the prescription, if needed. Smaller prescriptions mean that fewer painkillers sit unused in medicine cabinets.
“One of the things we have learned is that when people misuse these medications, they get them from family and friends who have leftover medication somewhere in their homes,” said Wilson Compton, MD, MPE, deputy director of the National Institute on Drug Abuse at the National Institutes of Health.
In addition, Orlowski cited the need for continuing research on how to adequately control pain without opioids. “Many academic medical centers have embarked on a process to treat chronic pain ‘opioid free,’” Orlowski said. “These trials will lead to improved care and understanding of how best to treat pain.” Alternatives to opioids may quell chronic pain without the danger of addiction. Options range from NSAIDs like ibuprofen to treatments such as acupuncture, mindfulness training, and massage, although the effectiveness of many treatments is still unproven.
Addiction: “You can’t tell”
Just about every medical center is devoted to reaching practicing physicians on addiction issues, said Orlowski. “Almost everyone that I’m talking to has ongoing programs.”
Among the programs are addiction medicine fellowships—44 in the United States approved by the Addiction Medicine Foundation and “more in the making,” said Lembke. The American Board of Medical Specialties recently recognized addiction medicine as a multispecialty subspecialty to allow physicians to apply for the new certificate. Any type of doctor who has completed residency can spend an additional year learning clinical addiction medicine. Compton said this opportunity may help ensure that “there are specialists to provide the ongoing support for complicated cases.”
Yet no amount of preparation—of doctors or patients—will remedy the willful deception by opioid addicts, she stressed. “Without objective data points, doctors struggle to know which of their patients may be misusing or addicted to prescription opioids. I’ve been treating people with addiction for years,” said Lembke. “I feel like I read people pretty well, and I can’t tell.”
But physicians can increase the use of objective data points currently available to them, such as urine tests and the consistent use of a prescription drug monitoring program to determine if addicted patients are shopping from doctor to doctor for painkillers.
Putting practices to work
At the University of Kentucky, Phillip Chang, MD, chief medical officer at UK HealthCare, has developed protocols that involve trying nonopioid painkiller regimens before prescribing opioids. Emergency physicians are trained to give greater weight to the long-term dangers of opioid prescription. The results have been so encouraging that Chang says that several health systems in Kentucky have shown interest in incorporating these protocols into their own guidelines.
At Boston Medical Center, Karen Lasser, MD, MPH, associate professor of medicine and public health at Boston University Schools of Medicine and Public Health, has conducted a trial of nurse care management, patient registry, electronic tools, and face-to-face meetings with doctors (known as academic detailing) to improve adherence to opioid monitoring guidelines. The study employed monitoring strategies, including a controlled substance agreement, urine testing, frequent visits, pill counts, and the use of state prescription monitoring programs.
“Primary care providers are overworked. There are a lot of guidelines providers need to be on top of—cholesterol guidelines, depression guidelines, back pain guidelines. The number of guidelines has exploded. That’s why we introduced this interdisciplinary model—so that it’s more of a team effort. You have the nurse tapping you on the shoulder: Hey, let’s order some urine testing for your patients,” Lasser explained.
“The intervention increased the proportion of patients who had treatment agreements, who had regular urine testing done to monitor them while they were on opioids. And it actually increased the rate at which patients were terminated from opioid prescriptions, and it led to lower opioid doses,” Lasser said, although pain levels weren’t tracked in the trial.
If strategies to prevent addiction fail, doctors also need to recognize that addiction treatment, though difficult, can be effective, Lembke stressed, “It’s one of the great myths that addiction treatment doesn’t work. It really has about a 50 percent response rate, which is on par with the response rate to other chronic illnesses, from Type 2 diabetes to major depression.”
