When the first vaccines for COVID-19 were shipped to states in December 2020, West Virginia’s public health officials were prepared. Health systems began immediately vaccinating front-line health care workers, and clinics were set up across the state to vaccinate any health care workers who were not part of a larger hospital system. Almost 250 local pharmacies were tapped to vaccinate residents and staff at the state’s nursing homes and assisted living facilities — and had completed the first round of shots in all of its facilities by the first week in January. Next up were residents age 80 and older and K-12 teachers age 50 and up.
Indeed, for the first few months of the vaccination rollout, West Virginia led the nation in protecting its most vulnerable residents. Like many states, though, in recent weeks West Virginia has found its early vaccination success running up against resistance from a significant number of residents who don’t want the vaccine or want to wait and see.
At the end of April, West Virginia Gov. Jim Justice announced a new campaign to tackle this resistance. For young people ages 16 to 35, the state is offering $100 savings bonds. For rural residents who live far from cities — the majority of West Virginians — the state is mobilizing mobile clinics to bring the vaccines directly to the people. And for those residents who don’t trust government-run clinics but who do trust their doctors, several dozen primary care providers will begin offering the vaccines at doctor’s offices in the next few weeks.
AAMCNews spoke with West Virginia Health Commissioner Ayne Amjad, MD, MPH, about why early efforts worked so well and what initiatives the state will be launching in the coming weeks.
What elements were key to the early success of your vaccination program?
 Courtesy Ayne Amjad, MD, MPH
Courtesy Ayne Amjad, MD, MPH
In the beginning, we set up an interagency task force with all of our stakeholders, so we had one representative from our long-term care facilities, our hospital associations, our patient and community care clinics all under one roof. And then those representatives brought information back to those stakeholder groups to decide what was best in getting the vaccines to those communities.
West Virginia was the only state that opted to use local pharmacies — rather than CVS or Walgreens — to vaccinate its long-term care residents. Can you talk about that decision?
Well, we don’t have a Walgreens or a CVS on every corner in West Virginia. But the mom and pop chains have been here 40 years, some of them, and they are embedded in our communities and have long-term relationships with our long-term care facilities and their residents. During the initial vaccine rollout, we had one pharmacist who lost a family member, and we offered to go in and finish the vaccination process for his long-term care facilities. But the pharmacist said no, he just needed one day off to take care of some family business and then he wanted to finish vaccinating the residents because he had relationships with them. He had provided medicine for them for so long. In West Virginia, most people trust their pharmacists, just like they would their doctors.
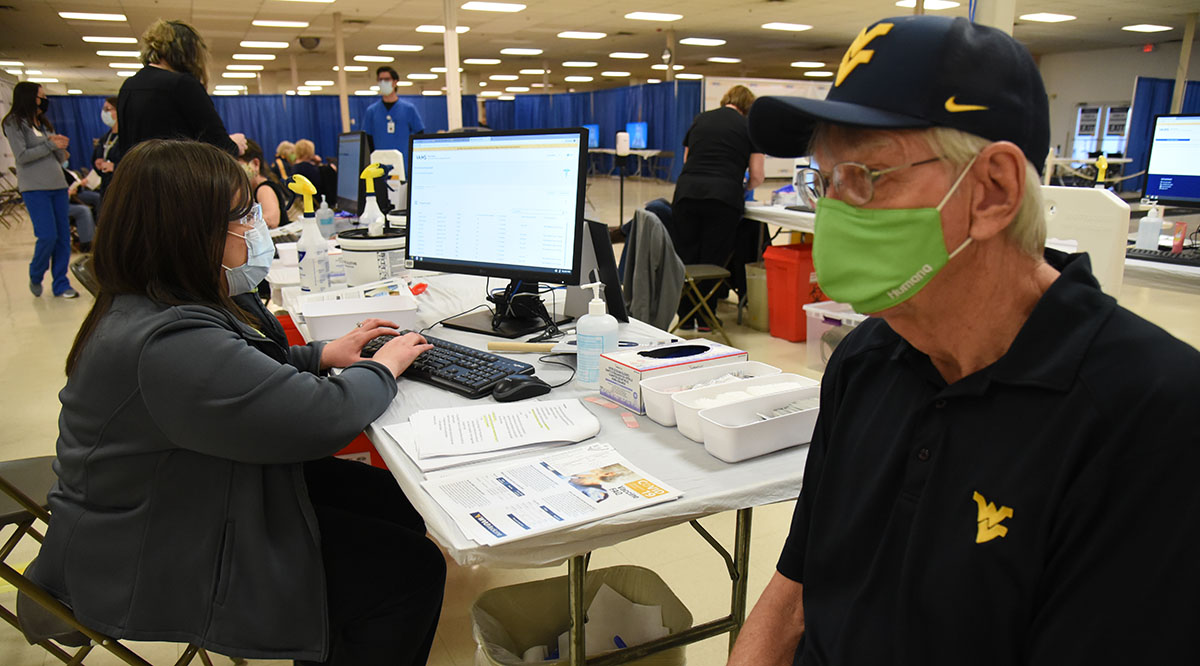
West Virginia also set up large clinics, but you didn’t call them mass vaccination clinics. Why was that?
We have a great team at West Virginia University that does a lot of research, and they did focus groups before the rollout in December to decide how best to get vaccines into arms. One thing they discovered is that the idea of a “mass clinic” did not resonate with the people of West Virginia. Initially, we told people to avoid mass gatherings, to not go where there were large numbers of people. Instead, we found the phrase “community-based clinics” or “community-based approaches” worked best. We used #CommunityImmunity a lot. We wanted people to think about your community and get vaccinated not just for yourself but for other people.
In a rural state like West Virginia, how do you get vaccines out to people?
Initially, we had community clinics around the state, and we used our local health departments too. But then we had mobile units that were able to get to more rural areas.
We also have a lot of partnerships within those communities. Our health departments partner with community members and pharmacists who can get to these rural pockets of the state. It’s people knowing people — sometimes, you wouldn’t even know that the road was there if you didn’t live there.
Like many states, West Virginia now has more vaccine supply than demand. What are some other measures the state is taking?
Just this past Monday, our governor announced a plan to give $100 savings bonds to 16- to 35-year-olds, because that’s the group that we’re seeing doesn’t want to get vaccinated. That’s also the group where we’re seeing the greatest number of variants, among the 16- to 40-year-olds. Some people say, “Why savings bonds?” But it’s an investment in your future, just like the vaccines are an investment in your future. We want them to be a part of this initiative to end the pandemic.
It is hard, and sometimes, you have to give people time and understanding and let them come to that conclusion by themselves after they get more information. In time, I hope we have more people coming to get their shots. We are seeing people trickle in every day, and every person who gets it is a positive sign to me, so we’ll take it.
What are some of the concerns that you’re hearing from those who weren’t part of that first group that was eager to get the vaccines?
Some people were waiting to see if co-workers got sick from [the vaccines]. People just didn’t want to have any side effects. Or they wanted to see more news media coverage come out.
Then there are a lot of people who just didn’t have the time to get it before, or the access to it, or they didn’t think there was a rush to get it. The 30- to 50-year-olds thought, “Oh, there’s no big rush to get it, I’ll just get it when it gets here.”
Some people say they want to get it from their primary care doctor. We’ve already signed up 70-plus providers, and we’re going to try to push it out to more providers. Primary care physicians, pediatricians, family doctors are probably the most trusted sources in our communities, so we’ve been onboarding those providers for some time now and we’re getting ready to push the vaccines out to them in the next week or two. Some patients preferred getting the flu vaccine in their doctor’s office as well, rather than going to the pharmacy. They just felt it was safer or better.
Some people are really adamant about not getting a vaccine. When you talk to those people in your state, what are they saying?
There’s a belief, especially among young people, that it causes infertility, which we know is not true.
The next one is people believe that it’s somehow going to mess up their DNA, because they hear it’s a messenger RNA vaccine.
And the next one is that younger people believe they will get over COVID and there’s no problem with long COVID symptoms and they will be fine. Those are the main issues that we’re hearing.
I practiced primary care for 10-11 years before taking this job, and I’ve dealt with people who don’t want to take their diabetes medicine or their high blood pressure medicine. I’ve discharged patients who are noncompliant, and I’ve taken patients back who are noncompliant just because I like them.
For someone who doesn’t want to take the vaccine at this stage — well, there are people I would want to insist, you know, if they are really old or they live in a long-term care facility. But if there is a young person who is so resistant, I’ve dealt with enough patients to know that the more you push them, the more they won’t do it. And maybe they need more time to see the benefits for themselves. Maybe they need to see more data. We just try to provide as much education as we can, give them the most sound information. Sometimes they just want to be heard. And you pick people who are trusted in the community to talk to them.
We have patients who have refused the vaccine and then gotten sick and are begging for the monoclonal antibodies. And we give it to them. That’s what we do.
I’m really proud of what we’ve accomplished, not just with the vaccines but with the virus. People are wearing their masks; that’s not an easy thing to accomplish. We’ve done pretty well with our numbers. I think we just need to hunker down a few more weeks and vaccinate as many people as we can.
