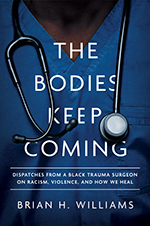
Editor’s note: The opinions expressed by the author do not necessarily reflect the opinions of the AAMC or its members. This essay is adapted from The Bodies Keep Coming: Dispatches from a Black Trauma Surgeon on Racism, Violence, and How We Heal by Brian H. Williams, MD.
Conventional wisdom in trauma surgery is that gun violence is worse from Memorial Day to Labor Day. In the gallows humor that bonds trauma surgeons, “Shooters polish their guns for the summer, and lock ‘em up for the winter.” It is a trope I’ve heard countless times, one I’ve often repeated. But with over two decades in medicine, I’ve learned the lethality of bullets is not seasonal. Black people are gunned down year-round.
In treating these patients, I see myself. In comforting their families, I see mine. A few years from now, my cousin will be shot and killed in front of her three young children. For me, working to end the epidemic of gun violence is more than an academic pursuit or my vocation. It is personal.
“Doctor, please take me to see my boy.” The mother is grasping fistfuls of my white coat. On her knees, she pleads with me, then the heavens, back to me, back to the heavens. She releases her grip, leaving wrinkled, dusty handprints. “I lost my oldest last year; now this. Lord, why you do this to me?” It is less a question and more a tortured reproach. I want to take her to see her son [Malik] but I can’t. His body is a crime scene, evidence to be preserved for his post-mortem examination, the autopsy.
The chaplain eases beside me. “Thank you, Dr. Williams. I’ll take it from here.” Her timing is perfect, for there is nothing more I can do. My expertise is medical, not spiritual. “Again, I’m so sorry for your loss,” I say [to the mother]. “Here’s my card. I’m here all night if you think of any questions.”
Few mothers ever call me. Like I do on every trauma shift, I move on. The trauma team moves on. The hospital moves on. I must be ready for another victim, arriving by lights and sirens. I file away this mother’s son’s death in the emotional lockbox straining to contain the feelings of injustice for the countless others like him. In these moments I reckon with the role I play as a Black doctor in a society that devalues Black lives. I wrestle with the futile feeling that the nobility of my work does not have a sustainable impact. The essence of my job is plugging bullet holes in young Black men and women, at least the ones I can save — and then sending them back to an environment where they remain at high risk of reinjury and death.
What is it about these neighborhoods where I have worked that endemic violence persists in tandem with health inequity? What does it say about our nation’s values that we allow it to persist?
Nationwide, young Black men aged 15 to 34 represent 2 percent of the population but 37 percent of gun homicides. Some people call my patients victims of “Black-on-Black” violence, but I remind them: interpersonal violence is a byproduct of proximity and we live in a mostly segregated country. Since we have sorted ourselves into homogenous racial and ethnic neighborhoods, a result is that “white-on-white violence” occurs at the same rate, according to the U.S. Department of Justice. I also remind them Black men are fatally shot by police at more than twice the rate of white people, even though white men are more likely to be armed in the same scenario. And each year, more people are shot and killed by police than in all the mass shootings combined. The extremes to which America contorts its values to minimize all these deaths are untenable.
Malik, like hundreds of others, is merely another statistic for our hospital death registry. The national news will not cover his death. The local news might. If the mother does call me with questions, the most truthful answer I can give — the one internalized yet never verbalized during my 20-plus years in medicine — would be: Ma’am, your child is nothing more than another Black body that came to be tagged and bagged.
Nobody gives a damn.
Giving a Damn
Within a year of my move to Chicago [as the newly appointed surgeon to the Level 1 trauma unit at University of Chicago Medicine], the coronavirus pandemic began ravaging the Southside Chicago neighborhood I served. Nationwide, the COVID-19 mortality rate for Black people was more than double that of white and Asian people, and a third higher than that of Latino people. In Chicago, more research by my colleagues found that “patients living in Black majority neighborhoods had two times higher odds of COVID-19 positivity relative to those in white majority neighborhoods.” Once again, I had a front row seat to death and healthcare inequity, replicated in impoverished Black communities across America, being accepted as business as usual.
Even as these tragedies unfolded, I awakened each day energized, knowing my job had purpose. I was part of a team saving lives, comforting families, and teaching trainees. For a trauma surgeon like me, who thrives on adrenaline, it was a dream job.
Yet questions continued to plague me. Did my work have a sustainable impact? How could I participate in an unjust healthcare system that was part of the problem? Were my patients better off after I cared for them than they were before?
During the early years of my career, saving the life of a gunshot victim — or trying to — was exhilarating. And the more gunshot victims the better. But now I kept thinking: by the time patients are lying on the gurney in front of me, it’s too late. I might be able to save them from immediate death, yes. But what about the circumstances that led them to my trauma bay? What about the forces that shape where they live, work, learn, worship, and play? What access to transportation and banks and grocery stores and parks do they have — or not have? Did my work as a trauma surgeon truly help transform the communities I served? The answer I felt was a resounding no.
Bound Together
[I began to see,] in more vivid detail than ever before, that the Black bodies on which I worked were imprisoned within transgenerational systems designed, from the start, to restrict the pursuit of life, liberty, and happiness. In fact, I saw that the systems around us — of healthcare, housing, education, economic opportunity — weren’t actually failing. It only seemed like they were. In fact, they were working exactly as they had been designed: to advantage some people and disadvantage others. I still didn’t know exactly how those systems functioned, but I knew I had to learn. I had to understand how they interacted with the healthcare my colleagues and I provided. And the idea gave me a modicum of hope, which is sometimes just enough to get through the day.
“America began with a great paradox: the same men who came up with the radical idea of constructing a nation on the principle of equality also owned slaves, thought Indians were savages, and considered women inferior,” writes historian Heather Cox Richardson in How the South Won the Civil War. “This apparent contradiction was not a flaw, though; it was a key feature of the new democratic republic.”
Richardson’s point — that sometimes what we believe to be flaws of a system are actually features — now informed my perception of healthcare in the United States. It informed my view of everything, really. The reality that systems produce the results they’ve been designed to create illuminates so much about our country. If racism is not a bug, but a feature of our common life, I knew we had to do more than nibble at the edges. As imperfect as our shared history is, we can use the knowledge of our past to understand our present and create a better future. Despite the flaws of the authors, the words in our Declaration of Independence and Constitution are still ideals toward which we can, and should, strive.
But to achieve this, we must hold these dichotomous truths to be self-evident. America is a great nation born from genocide and chattel slavery. Many of our founding fathers championed both racism and equality, slavery and freedom. And the seeds of our history, while creating the greatest democracy the world has ever known, grew roots that permeate all aspects of our society: seen and unseen, good and bad, triumphs we praise and mistakes we ignore. At some point the past has to be the past, yes. But any future greatness America attains will not happen by ignoring, rewriting, and excusing our shared history — but by affirming it.
The problems of healthcare disparities and racism in medicine are not limited to a once-in-a-century pandemic. When admitted to a hospital, Black patients experience more adverse events than white patients. In reviewing patient safety according to 11 different indicators, a report by the Urban Institute and Robert Wood Johnson Foundation found that “Black adult patients experienced significantly worse patient safety in six indicators when compared to white adult patients who were in the same age group, of the same gender, and treated in the same hospital.” These disparities occur more frequently in surgery, my specialty, than in some others.
By underinvesting in the health of poor and Black citizens, the infrastructure of the entire state suffers — which, in some way, impacts all of its citizens. And these healthcare inequities are connected to other types of injustice.
But here’s the thing: history is not inevitable. People in power make choices, and just because the United States now has massive health disparities does not mean that it had to be that way. Nor does it have to continue. That is why we must talk about structural racism and how it binds us all.
