Primary care physicians often struggle to connect patients with specialists. Specialists, on their end, are often overwhelmed by referrals. Five years after its launch, the AAMC's Project CORE has helped improve patient care for more than 2 million patients.
When a primary care physician (PCP) needs a quick answer from a specialist, the informal curbside consult is usually the go-to option. But what if a specialist isn’t readily available, or a patient lacks the time or money to meet with a specialist should a follow-up be needed? And what should the PCP tell the patient in the meantime?
These are all common challenges in the patient-PCP-specialist communication loop that the AAMC’s Project CORE (Coordinating Optimal Referral Experiences) successfully tackles.
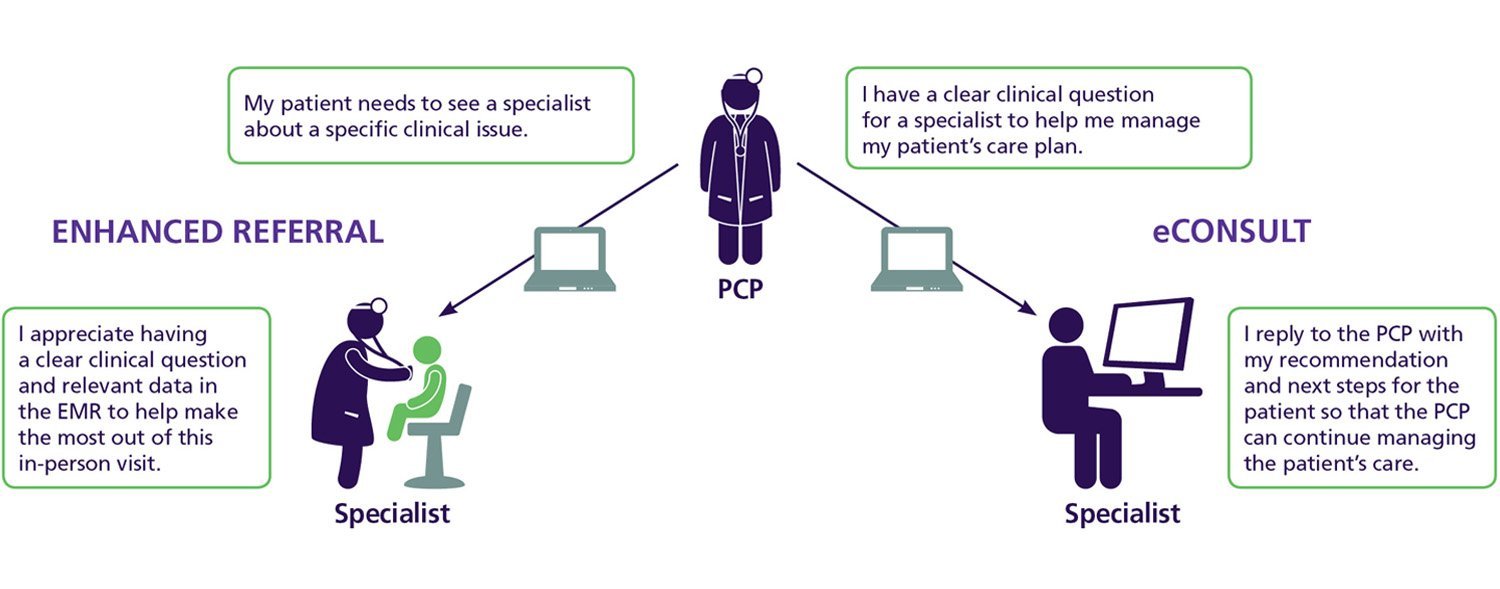
Now in its fifth year, Project CORE is designed to improve care coordination between PCPs and specialists. The model uses two key elements — enhanced referrals and eConsults embedded in the electronic medical record (EMR) — to facilitate more efficient, effective communication between them.
Using an eConsult, PCPs can quickly determine the best course of action with the guidance of a specialist. And should a patient need to see a specialist in person, that provider is equipped with an enhanced referral based on a specialized template full of information that helps ensure the visit is most effective in meeting the patient’s needs.
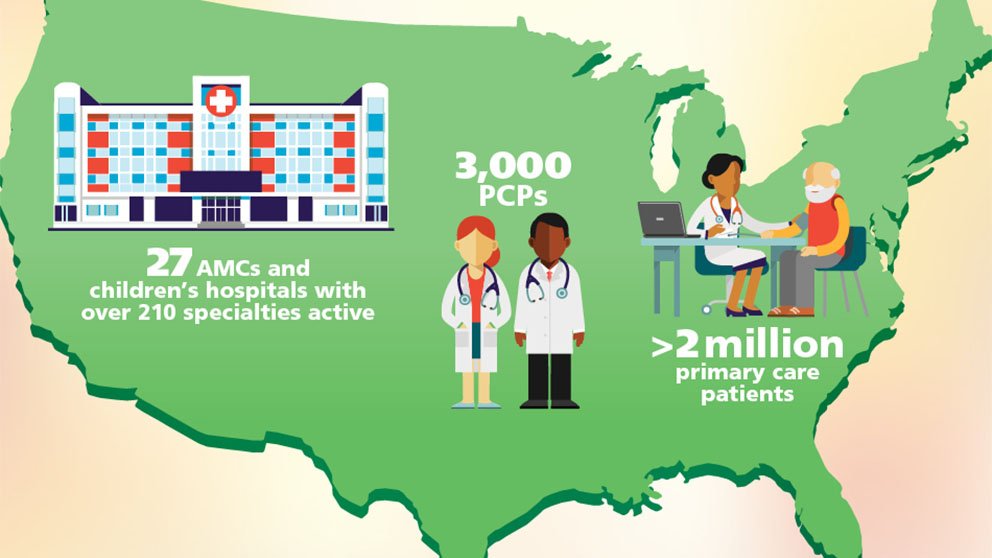
In its first three years, Project CORE’s participating institutions experienced an 84% increase in timely access to specialty care and avoided an estimated 7,360 unneeded specialty referrals. As of 2018, the program has been implemented at 27 institutions where more than 2 million primary care patients can benefit from the model. Initially funded by a Center for Medicare and Medicaid Innovation award, the program continues to grow, with a new collaborative of academic medical centers launching this year.
These are some of the ways that enhanced referrals and eConsults are changing medical practice for the better:
1. Higher-value in-person visits
Making the trip to visit a specialist can come with a host of challenges for patients. “The time and effort by the patient just to come in to see the specialist is not trivial,” from taking time off work to finding adequate parking at the medical center, says Anne Fuhlbrigge, MD, MS, associate dean for clinical affairs and executive sponsor for CORE at the University of Colorado Health. That’s particularly important for patients with limited mobility or other barriers to accessing care.
“There are definitely providers who, for their patients that are paying out of pocket, almost always start with the eConsults instead of referrals just because it is much more cost-effective if the patient doesn’t need to see the specialist” in person, says Kim Dowdell, MD, primary care lead for CORE at the University of Virginia Medical Center.
2. Streamlined communications
Academic medical centers are full of busy people. Having a system in place that brings primary care providers and specialists together via a digital platform can help simplify communications.
“We have a large academic institution with multiple satellite clinics where most of the primary care physicians are actually not at the main hospital,” says Julia Chen, MD, primary care lead for CORE at the University of Michigan. “As a result, there can be some barriers to communication between specialists and primary care physicians in knowing each other and collaborating. The eConsult program and CORE program has helped to improve that communication.”
And with better communication in place, PCPs can provide better continuity of care and more comprehensive care for their patients.
“The eConsult is a way to help provide guidance back to the PCP for those cases that can continue to be managed in primary care,” says Meaghan Quinn, MHSA, program manager for Project CORE at the AAMC. “With more timely specialty input through the eConsult tool, they can maintain continuity of care for the patient in their primary care medical home.”
3. Shorter wait times
Specialists are often inundated with appointment requests, which can lead to weeks-long or even months-long wait times for patients seeking their expertise.
“As is true of many health systems, there can be long wait times for some specialties,” says Chen, who points to dermatology as one example. Whereas it may normally take months for a patient to see a dermatologist in person, that time is cut significantly when a dermatologist can quickly assess a photo of a rash or skin lesion. PCPs can often get a response from the dermatologist within a few hours, notes Chen.
Under the CORE model, PCPs typically hear back from specialists within a day, and almost always within 72 hours.
“[Patients are] excited to get an answer back quickly and then be able to either move on in the diagnostic process or start treatment without having to wait for an appointment,” adds Chen.
4. Better documentation
The CORE model provides point of care decision support that enables better communication between providers. Condition- and specialty-specific templates in the EMR prompt PCPs to detail their expectations for care and help them determine next steps.
“Having something that's officially documented in the chart is always better than something that's unofficially documented or summarized,” with PCPs retaining a record of specific instructions from a specialist, says Dowdell.
“The specialist who's answering the eConsult is someone who has opted in to be the eConsultant and they've been trained on how to write a good eConsult response,” notes Quinn.
5. Improved access to specialty input
CORE allows patients with low-acuity, low-complexity problems to get their issues addressed quickly and efficiently, freeing up specialists’ office time to focus on those who need more complex care. “The majority of eConsults can be managed without an in-person specialty visit, freeing up space for other patients that are also trying to access the clinic,” says Quinn.
The model can also help physicians to prioritize patients in need of more timely or intensive services by specialists. With more direct communication between PCPs and specialists, they can more effectively triage patients to the right provider at the right time.
“The specialist could pick up something that could improve patient safety and outcomes because they are more attuned to that [clinical problem],” notes Fuhlbrigge.
Interested in learning more about Project CORE? Visit www.aamc.org/projectcore.