In Kalamazoo, Michigan, infants of color are four times more likely than white infants to die before their first birthday. That striking disparity in infant mortality is rooted in socioeconomic status, racism, and other social determinants of health, local community health leaders say. But a burgeoning partnership between several community health organizations and Western Michigan University Homer Stryker M.D. School of Medicine (WMed) is not only shrinking the gap, but also providing better care to women and their families.
The joint project, known as Cradle Kalamazoo, is one of nine programs at teaching hospitals and medical schools made possible through an AAMC initiative funded by the Agency for Healthcare Research and Quality. That initiative, “Building a Systems Approach to Community Health and Health Equity for Academic Medical Centers,” has helped these nine institutions strengthen partnerships with local organizations and better coordinate their internal community health and health equity programs.
“The idea wasn't necessarily to spark new community partner activity, but to really get our institutions to think more systematically about how they could reduce redundancies, increase efficiencies, work together, and collaborate more, both internally and externally, so that the work they were already doing was maximally impactful,” says Philip M. Alberti, PhD, AAMC senior director of health equity research and policy. In fact, all institutions were required to include a public health partner and community health partner on their teams.
As the three-year pilot enters its final phase, the health equity systems cohort members are celebrating their successes and determining how to continue elevating community health issues.
Here’s a look at what four of these institutions have achieved across wide-ranging areas, from reducing disparities in infant mortality to improving diabetes care, preventing concussions, and promoting C-suite focus on issues of health equity.
Supporting moms, saving babies
To improve women’s access to care and reduce disparities in infant mortality rates, Cradle Kalamazoo identified four areas of concern: safe infant sleep, reproductive health, the need for perinatal home visits, and a recognition that cultural humility should be integrated into the other priority areas.
“[The] grant allowed us to specifically look at the health equity concerns of the community and find out more about where we could partner as an academic institution.”
Cheryl Dickson, MD
Western Michigan University Homer Stryker M.D. School of Medicine
“[The] grant allowed us to specifically look at the health equity concerns of the community and find out more about where we could partner as an academic institution,” says Cheryl Dickson, MD, MPH, associate dean for health equity and community affairs at WMed and lead researcher for Cradle Kalamazoo. “Specifically for Cradle, we were able to add a component not being looked at that impacted disparities in infant mortality related to women of color having early access to prenatal care.”
Being directly involved in the community has helped Cradle Kalamazoo members understand the barriers that families face in raising healthy children, she adds. “It needed to be culturally responsive to make a difference for what we’re seeing in the disparity.”
Subcommittees at WMed affiliates Bronson Healthcare and Borgess-Ascension Health are looking at challenges that black women in particular encounter when accessing health care. For example, to ensure responsiveness, hospitals are assessing how long it takes for women to get appointments and how they are processed through the system.
Cradle Kalamazoo is also working to provide women with free pregnancy tests and connect them with community health workers in clinics, with early entry into prenatal care if their pregnancy tests are positive. Resources are available for women after delivery as well.
As a relatively young medical school, established in 2012, WMed has the opportunity to create new partnerships to advance health equity, says Dickson.
“My role is making those connections in the community, creating partnerships that work for both, and really looking at what are the concerns of the community regarding their health, and what a medical school can do — so it's actually a win-win,” she notes.
An impact on concussions
Youth football is a popular pastime in Mississippi, making concussions a significant public health concern. Yet too often, low-income and rural athletes have trouble accessing the concussion care they need.
Through Heads Up Mississippi, the University of Mississippi Medical Center (UMMC) is helping create a statewide, coordinated concussion effort featuring a collection of vital data and better medical management. Heads Up Mississippi also seeks to educate community members, from athletic coaches to players and their families, on the health consequences of concussions.
“We have the opportunity to do something truly unique because of the environment in Mississippi that we're working in, that we’ll be able to impact this population health need across the state in a very different way, by using an evidence-informed approach,” says Jennifer Reneker, PhD, PT, MSPT, associate professor of population health science at UMMC.
“To really engage with the community means not going and telling them what we're going to do. [Rather, it involves] talking to them about how we can help and ... spending time with them.”
Jennifer Reneker, PhD
University of Mississippi Medical Center
Getting specialist care in a state as rural as Mississippi can require a long trip, so UMMC is working to create a centrally located institution that people can reach more easily. As a Health Resources and Services Administration National Telehealth Center of Excellence, UMMC is also exploring ways to optimize telehealth for concussion care.
In addition, UMMC is working to connect with local groups in Jackson, Mississippi, where it's located. “To really engage with the community means not going and telling them what we're going to do,” says Reneker. Rather, it involves “talking to them about how we can help and ... spending time with them.”
Developing a concussion management system is now that much closer to becoming reality with the support of upper-level administration and many passionate partners, says Reneker.
“What I think the [initiative] has really done is provided that impetus to not let it sit on the back burner, and to keep it in our vision,” she notes.
Visiting diabetes patients in their homes
A partnership to address diabetes and related conditions was a natural fit for Baylor College of Medicine (BCM) and Harris Health System (HHS). The institutions both focus on community service and delivering quality health care, and HHS already had a pilot diabetes program, notes Toi Harris, MD, associate provost of institutional diversity, inclusion, and equity and student services at BCM.
“Our location in the Texas Medical Center in the heart of the city really is an excellent opportunity to collaborate [with] other institutions to improve the health of those in our community,” she says.
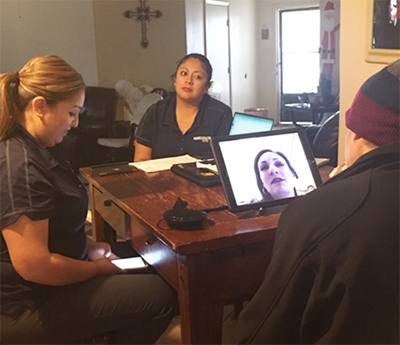
The BCM-HHS team implemented a community health worker program to make home visits with patients from seven HHS community clinics, educating patients and connecting them to additional resources and support as needed, including referrals to nutritionists and mental health providers. Patients in the program have experienced decreases in hemoglobin A1C levels and improvements in their diabetes knowledge, says Harris.
But patients aren’t the only ones getting an education: staff, medical professionals, and affiliate providers also are all learning about social determinants of health that influence diabetes and related conditions like heart disease.
"Convening people from different professions ... as well as people across the continuum from students to faculty to staff ... helps inform the overall approach to improve the success rate of meeting our project’s aims,” says Harris.
Working in the community and the C-suite
With dozens of community health and health equity initiatives taking place at Vanderbilt University Medical Center (VUMC), the institution needed to take stock of all its related programs and determine how to align them.
A first step was creating a centralized office for health equity. In January 2019, the university also appointed Consuelo H. Wilkins, MD, MSCI, a recognized leader in community engagement, as vice president for health equity at VUMC and associate dean for health equity at Vanderbilt University School of Medicine. Initially, the office is focusing on three pillars: community and population health improvement, health equity research, and health equity education and training.
Wilkins says the office is committed to ensuring that staff working on health equity get necessary support. “We want to make sure that we understand what their needs are, their perspectives, and how we can make them want to come to us to provide information and share their work and how they’re functioning,” she says.
The AAMC initiative “required us to bring together leaders representing different areas across the enterprise to have critical discussions about health equity,” says Wilkins. Also, “the program enabled us to quickly and strategically develop and implement plans for achieving our goals by providing resources and tools such as the health equity inventory, protocols for gathering stakeholder input, and evaluation templates.”
Indeed, the institution is so committed to health equity that it’s exploring how to link performance goals to some C-suite bonuses, she says.
Changes aren’t just happening on the inside. Building trust through better community engagement has been central to the initiative, notes Wilkins. For example, VUMC staff visit sites such as community health clinics and health departments to partner with local leaders on solving problems. “We have made a lot of efforts to go to community tables as opposed to only inviting community members and partners into academic institutions,” Wilkins says.
Sustaining health equity efforts
Now two years into the health equity effort, the AAMC is working to help cohort members plan for the future of their projects and identify ways to help spread the program’s benefits.
Throughout the initiative, the AAMC has brought teams together for regular meetings to discuss setbacks and successes. The group has also worked to create helpful resources, such as a database institutions can use to collect and search all their equity-related programs. Now the goal is to develop a toolkit that other academic health institutions can use to bolster their equity efforts, says Alberti.
In addition, the AAMC is working to help cohort members identify new funding streams once the pilot ends. Strategies for sustainability will be the focus of a meeting on June 20 at AAMC headquarters in Washington, D.C., as members present plans for communicating with a range of stakeholders who may be interested in providing funding. They’ll also hear from potential funders, such as health insurers and venture capitalists, who will offer insights into crafting their messages.
“There is a lot of hunger for doing this work,” says Alberti. “So, let’s push it forward.”
