When Melvina L. McCabe was in an eighth-grade boarding school, she told a teacher she wanted to be a doctor. The teacher replied, “You know what, Melvina? I think you’d make a better dental hygienist.”
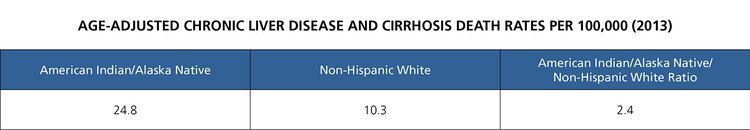
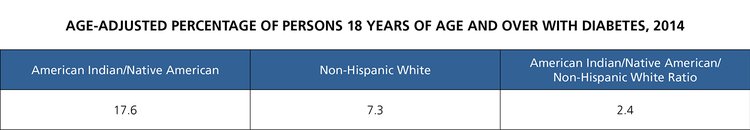
McCabe didn’t follow that advice, though, and is now Melvina L. McCabe, MD, associate vice chancellor for Native Health Policy and Service at the University of New Mexico Health Sciences Center. At the AAMC seminar “Advancing Health,” held in July 2016, McCabe discussed health inequities in the American Indian and Alaska Native community. The U.S. Indian Health Service (IHS) has documented that these populations suffer disproportionately from heart disease, intrahepatic bile duct cancer, diabetes, alcoholism, mental health problems, asthma, and chronic liver disease.
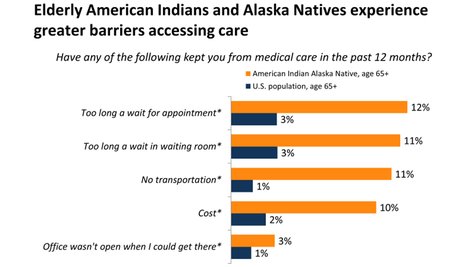
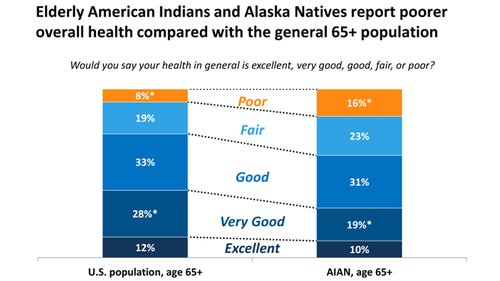 Kaiser Family Foundation, 2013
Kaiser Family Foundation, 2013
Poverty is at the root of many of these health disparities, McCabe said. About 28 percent of American Indians and Alaska Natives lived in poverty in 2014, compared with 15.5 percent for all Americans, according to the U.S. Census Bureau. The median household income for American Indian/Alaska Natives is $37,227, compared with the national average of $53,657.
Without money, people are less likely to have health insurance or seek medical care. Nearly one in four American Indians and Alaska Natives lack health insurance, compared with the 11.7 percent uninsured rate for the entire U.S. population. Annual per capita spending on health care directly through IHS is $3,099, whereas for the general population the figure is $8,097.
McCabe also linked poor health to limited educational opportunities. While 83.2 percent of Americans completed high school in the 2014-15 school year, just 71.6 percent of American Indians and Alaska Natives did, according to the U.S. National Center for Education Statistics. In addition, 19.8 percent of American Indians and Alaska Natives age 25 or older had a bachelor’s degree or higher in 2014, compared with 32.5 percent of all adults.
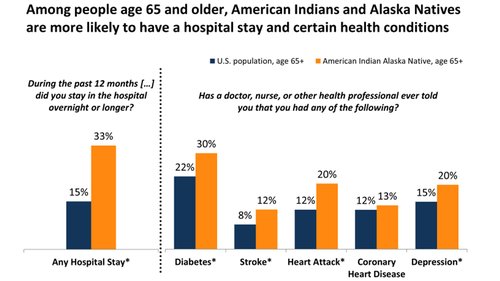 Kaiser Family Foundation, 2013
Kaiser Family Foundation, 2013
“Think of the effect of income on the ability to achieve health education,” McCabe said. Low-income and uninsured people lack the means to afford quality health care. And those who lack higher education are likely to lack the knowledge to make informed decisions about health care.
Wanted: More American Indian/Alaska Native physicians
Still another factor in American Indian and Alaska Native (AI/AN) health disparities is a shortage of AI/AN physicians and other health care professionals. Having familiarity with the cultural values, lifestyles, and spiritual beliefs of a patient can enhance the doctor-patient relationship. Physicians with knowledge of and sensitivity to the traditions of these communities can improve the health care that is delivered, noted Aaron Robinson, MPH, president of the Association of Native American Medical Students and a fourth-year medical student at the University of Wisconsin School of Medicine and Public Health.
“It's a careful balance of practicing medicine while respecting culture and belief, whatever that may be.”
Aaron Robinson, MPH
University of Wisconsin School of Medicine and Public Health
American Indian and Alaska Native physicians can communicate with AI/AN patients in ways that others may not be able to, Robinson explained. “It’s all about personalized care to the patient and making sure that the patient is getting healthy but at the same time molding your practice to [the patient’s] desires that fit [the patient’s] lifestyle and beliefs,” said Robinson, who has participated in traditional healing ceremonies. “It's a careful balance of practicing medicine while respecting culture and belief, whatever that may be.”
Finding strategies to increase the number of American Indians and Alaska Natives in medicine is imperative. “If we keep going as we are, we’re going to bottom out,” said Robinson. In 2016, 553 AI/AN students applied to medical school, but only 194 of those applicants enrolled—a decrease from 202 AI/AN enrollees in 2014, according to new AAMC data.
“Effective recruitment and retention of American Indians and Alaska Natives into medicine and other health careers to increase our numbers are paramount,” said Mary J. Owen, MD, director of the Center of American Indian and Minority Health at the University of Minnesota Medical School.
Given the low number of American Indian and Alaska Native enrollees in medical schools, positive examples and role models are sorely needed, Owen continued. “When I decided to go to medical school, none of the people in charge were Alaska Natives. There were no Native doctors, and very few Native nurses. [American Indians and Alaska Natives] were answering phones and mopping floors. I think we need to be represented at all levels and we’re not.”
Filling the gap
Rear Admiral Sarah Linde, MD, acting chief medical officer at IHS, noted the agency offers opportunities for doctors to work with tribal practitioners and healers. “It can be a very culturally rich experience,” she said.
She also pointed to recent programs to get more American Indians and Alaska Natives into health profession careers and improve health care delivery to these populations. One program provides up to $20,000 a year to repay qualifying school loans in exchange for a two-year commitment to work at an IHS facility that needs staff.
Linde noted that IHS is also working with the Health Research and Services Administration’s National Health Service Corps, a program which offers up to $50,000 in loan repayment in exchange for a two-year commitment to practice in a medically underserved community. Since 2011, all IHS sites have qualified for the program, and the number of participating clinicians has grown to about 400, Linde said.
The Association of American Indian Physicians (AAIP) is another national organization that advances excellence in Native American education in the medical disciplines and provides leadership to improve health care for the American Indian and Alaska Native population. AAIP offers educational programs and services to motivate AI/AN students to pursue careers in the health professions and biomedical research. The organization also hosts forums on combining modern medicine and traditional healing to enhance health care delivery in American Indian and Alaska Native communities.
When Native professors and associates are visible, Native students are more likely to follow, Owen said about the future. “We don’t own our own health care yet. We’re getting there, [but] we’re only going to effect change once we are at all levels of the hierarchy.”