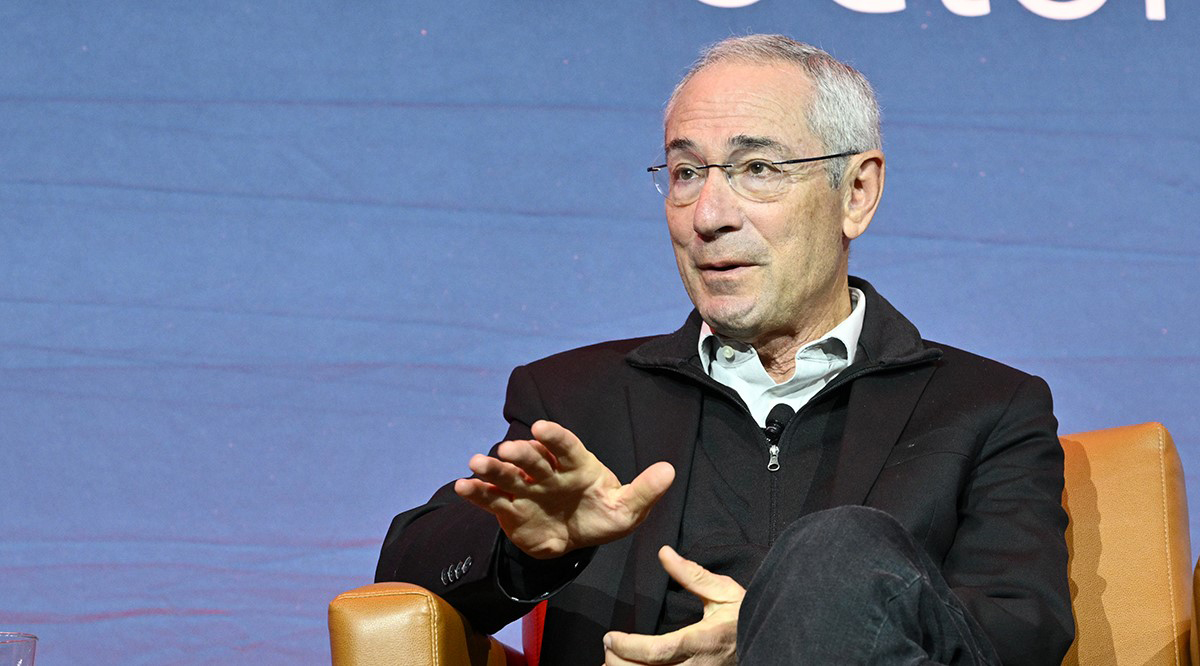
When he was working as the director of the National Institute of Mental Health, Thomas Insel, MD, a psychiatrist and neuroscientist, gave a speech to a public audience about the exciting advances happening at teaching hospitals in understanding the mechanisms of the brain.
Someone in the audience stood up and said, “Man, you just don’t get it.” He went on to explain that his 24-year-old son had schizophrenia and had been through several hospitalizations and jail stays, had attempted suicide, and was currently homeless.
“Our house is on fire and you’re talking about the chemistry of the paint,” Insel recalled the man saying.
It was a turning point in his approach to the mental health crisis that has plagued the United States and, despite advances in therapies and treatments as well as increased monetary investment, has continued to worsen over the past several years.
“That actually stunned me,” Insel said, speaking at Learn Serve Lead 2022: The AAMC Annual Meeting on Nov. 14 during a session entitled, “Healing: Our Path from Mental Illness to Mental Health.” “That’s the moment I thought, ‘Whatever we’ve been doing isn’t addressing the urgency of a public health crisis.’”
Because of the U.S. health care system’s failure to maintain an adequate mental health care infrastructure, even as medical advances reduce mortality for common physical ailments like cancer, stroke, and AIDS, “deaths of despair” – as a result of suicide, drug overdose, or alcohol use – have increased, Insel said.
“We’re up almost three- to fourfold from where we were at the turn of the century,” he said, adding that, for people under age 34, “deaths of despair” have killed nearly 15 times more people than COVID-19 has since January 2020.
The crisis is driven by five issues, according to Insel: lack of capacity due to the divestment of the federal government from mental health care infrastructure in the 1980s; lack of engagement, meaning people in need are not seeking help; lack of quality care; lack of accountability due to practically nonexistent data reporting; and equity issues that result in discrimination against those with mental illness.
But as dire as the current outlook is, Insel said that he has reason to be optimistic because there is evidence that these illnesses can be successfully treated, not only with therapy and medication, but with social supports that give people a purpose in life.
Insel proposes incentivizing the creation of systems that can help prevent people from getting to the point of crisis, which ultimately costs more in emergency department visits and hospitalization stays. He’s also encouraged by what he sees as the beginning of a shift in policy approaches at the federal and some state government levels.
“The answer, I think, is for us to begin to broaden what we mean by health care,” he said. “[And] to teach your students that what they need to think about is not simply what they're going to learn in the emergency room and on an inpatient unit, but about engagement. It's about figuring out how to meet people where they are … Yes, the problem is medical, but solutions are social, environmental, and political.”
Insel also emphasized the importance of the medical profession waking up to the mental health needs of its own workers, particularly medical students, who experience depression at a higher rate than the general public.
“Going to medical school isn't like being vaccinated against having mental health problems,” he said. “If anything [they] are higher risk, and we tend to tell our students that they need to be strong for everybody else. But we need to tell them that it's okay to not be okay. It's okay for them to seek help for themselves.”
Keep the conversation going
Discuss this session and more while networking with your peers in academic medicine during, and long after, Learn Serve Lead, by joining the AAMC’s virtual community. More than 3,000 of your peers are already there!
