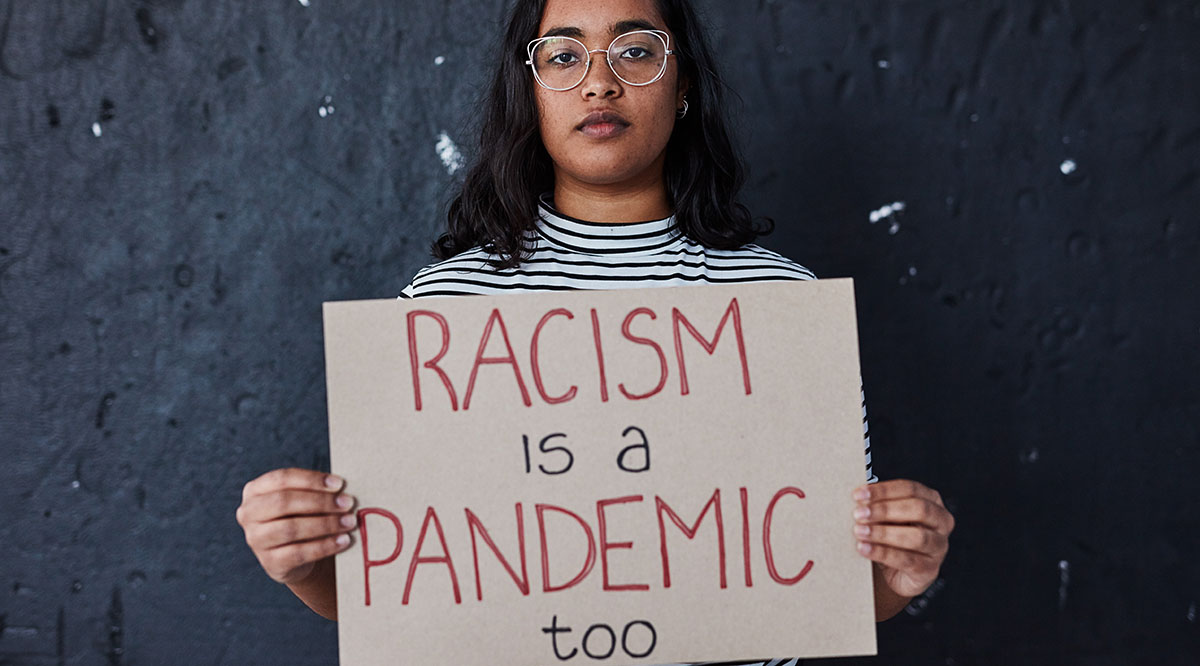
Citing the ongoing pandemics of COVID-19 and racism on the health of the nation, the AAMC (Association of American Medical Colleges) released a framework on Oct. 6 that is designed to guide and inspire the academic medicine community to begin addressing decades of structural racism within medicine.
The AAMC Framework for Addressing and Eliminating Racism at the AAMC, in Academic Medicine, and Beyond outlines four pillars of work that will guide the AAMC’s efforts “to create a shared vision of the AAMC and academic medicine institutions as diverse, equitable, inclusive, and anti-racist organizations.”
The four pillars include:
- Individual self-reflection on systemic racism and its manifestations in the workplace and beyond.
- Anti-racism efforts within the AAMC, including hiring an outside consultant to guide staff; establishing diversity, equity, and inclusion advisors within the organization; examining hiring, retention, and advancement policies; and holding staff accountable for racial inequities in the workplace.
- Anti-racism efforts within the academic medical community, including collaborating with academic medical centers to advance anti-racism efforts within medicine and advocating for change around health inequities affecting vulnerable communities.
- Anti-racism efforts within the broader community, including speaking out about racism; partnering with local community organizations to affect change in the Washington, D.C., region; and working with academic medical centers to help expand anti-racism efforts in their communities.
“Like many of you, I have felt increasingly distraught by the ongoing and repeated incidents of police brutality against those in the Black community, and by the struggles of my Black friends, neighbors, and colleagues who suffer on a daily basis from the historically dehumanizing and damaging effects of structural racism,” said AAMC President and CEO David Skorton, MD, in announcing the framework. “All academic medicine leaders — including the AAMC — must step up and transform rhetoric into action.”
AAMCNews sat down with Malika Fair, MD, MPH, an emergency physician and the AAMC’s senior director of health equity partnerships and programs, and Clarence Fluker, the AAMC’s director of community engagement, to talk about the impact of structural racism on providers and patients within academic medicine; why the time has come to address centuries of injustice; and what steps individuals, the AAMC, and academic medical institutions can take to become anti-racist.
Can you talk about the ways in which structural racism plays out in academic medicine?

Malika Fair, MD, MPH: I frequently witness racism in academic medicine. On a personal level, when I walk into a patient’s room, some of my White patients question my credentials. I get asked where I went to medical school and where I went to residency. I don’t see this happening to other physicians. Sometimes when I go into a room with a medical student or a resident who is White, the patient will talk to the student or the resident and not to me, even though I’ve introduced myself as the supervising physician.
I’ve also seen racism play out in patient care. It is not uncommon to see colleagues determine a diagnosis before they even see the patient, using generalizations about what a particular racial or ethnic group usually comes to the ER for. For instance, it is common to witness patients being labeled as “drug seekers,” “exaggerators,” or “drunks” without taking a complete history or doing a physical exam. By doing this, we can end up missing severe infections, injuries, or a new diagnosis by relying on the stereotype instead of asking the critical questions and examining the patient.
But racism in academic medicine touches every aspect of our work. It includes our inability to recruit and advance physicians of color; our failure to apply a holistic review to applications for medical school and residency; stereotypes that are still included in our curriculum; our insistence on using race in clinical algorithms, even though we know that race is a social construct and not a biological one; and our inability to give equitable care — there are still so many studies that show we are not giving analgesics to people of color who have a lot of pain.
Structural racism within the broader community also impacts health. Can you explain how that works?

Clarence Fluker: Institutional racist structures, systems, and policies have created social and economic conditions that lead to health disparities, poorer health outcomes, and lower life expectancies for Americans who live, work, and receive treatment at our academic medical centers. Washington, D.C., where I lead our community engagement work, is a microcosm of how these racist structures have contributed to poorer health outcomes and health disparities in our communities across the country. Right in our backyard, there has been a persistent and substantial Black-White life expectancy gap. The infant mortality rate for Black infants is four times higher than for White infants. The number of Black residents living with diabetes is seven times higher than for White residents. We also see a clear connection between race and homelessness in our community. Structural racism is made evident in our communities each day when we see the inadequate access to education, to housing, to quality health care leading to poorer health outcomes for Black, indigenous, and other people of color. Health equity is inextricably tied to racial equity.
Structural racism in medicine isn’t new. Why is there an urgency around addressing and eliminating racism now, in 2020?
Fluker: Certainly, COVID-19 illuminated to a lot of people the disparities that are happening in this country. Now more than ever, people have a wider understanding that health outcomes are closely linked to what’s happening outside of doctors’ offices and medical campuses, and that brings us to a greater understanding of the role that academic medicine can play in making substantive investments in change. But I attribute some of it to social media and people seeing things they might not have seen before, including the murder of George Floyd.
Fair: We have a window of opportunity where there’s a lot of attention on this topic. But it will not always be the case, because our nation has shown us before that we can acknowledge race issues and then somehow believe that they’ve gone away. We have to use this opportunity to make changes to the structures, policies, and procedures that contribute to racism in the medical community while we have national attention on this topic.
What does it mean to be anti-racist?
Fair: I define being an anti-racist as the conscious effort to express and act on ideals that promote racial equity and justice. This spring, we talked a lot about why Black and Brown communities were suffering in the pandemic and there was a lot of blame: blaming people of color for having chronic conditions, blaming them for unhealthy behaviors, for poverty, for their exposure to the pandemic. There was a lot of emphasis on something being wrong with people of color. We have to shift the conversation — and it is being shifted — to the impact of structural racism.
Fluker: Being anti-racist is not just a way of thinking, it’s a way of doing. As individuals, as an association, and as an academic medicine community, we must engage in anti-racism work and hold each other accountable for that work. We also must challenge our thought processes around this issue. In the same ways that racism has harmed so many people, there also has to be accountability from the people who have benefited from racism, whether intentionally or unintentionally. We rarely have the conversation about that. During the COVID 19 pandemic, the questions have often centered around, “What’s going on with Black and Brown people? Why are they getting so sick?” The parallel question is, “Why are others so well?” That starts the process of self-reflection for someone to say that “I am well because I have benefited from inequitable structures and treatment during my lifetime, and so I am better off than others.” People have been victimized by racism, but others have benefited, whether intentionally or not. Academic medicine has benefited from racism for centuries — for example, from medical research performed on enslaved people — and as a collective community, we have an opportunity now to acknowledge that and atone for that.
Why is it important for the AAMC to lead this effort, both individually and collectively?
Fair: It’s extremely important that we invest the time to understand our own biases, our prejudices, our power, and the imbalance of power that physicians have and how racism further worsens that imbalance. There is some self-reflection that has to happen as we embark on this work. We are hiring a consultant to help our association go through the anti-racism work that we need to tackle internally as we promote promising practices for our member institutions. We will also work with our partner organizations to see what our role in academic medicine is to address this in society and in our local community in Washington, D.C.
In many ways, our members are ahead of the game. We have students who have been passionate about this long before the pandemic and the murder of George Floyd who have already outlined what they hope happens with anti-racism in medical education. They are part of the catalyst for this work nationally. We have physicians across the nation who are experts in this. Our job is to make sure that we are aware of the most promising practices — that we convene experts, collect and promote these best practices, and provide a framework that is easy to understand and easy to act upon at our member institutions.
Is academic medicine ready to tackle the challenge of becoming anti-racist?
Fluker: A number of our members are well on their way to figuring out how they, as anchor institutions, can address racism and racial equity in their communities, from advocating for local policy changes to using their finances to reinvest back into the underserved communities in which their campuses are located to making sure that they are promoting local hiring, recruitment, and retention processes. The full power of academic medicine in anti-racism work isn’t limited to classrooms, hospitals, or individuals; the full power is in its ability to work in partnership with communities to achieve health equity.
Fair: We have a history of rising to the challenges facing academic medicine, whether it’s committing to the seven-plus years that it takes to train a physician, taking care of the sickest and most complicated patients, or discovering cures for the most formidable diseases. Racism is a challenge we have never risen to. But I think academic medicine is prepared to use our skills, our resources, the collective wisdom in our community, and the lessons our patients and partners can teach us, to tackle structural racism.
