As the COVID-19 pandemic enters its second year in the United States, many are eagerly awaiting their chance to get a COVID-19 vaccine. But among those waiting, the communities hardest hit by the virus are facing the biggest barriers.
Black and Hispanic people in the United States have been vaccinated at dramatically lower rates than their White counterparts — compounding the disproportionate impact COVID-19 has had on Black and Hispanic communities. As of March 2021, the share of Black people who were vaccinated was lower than their share of the total population in every state. Nationwide, although race was only available for about half of all vaccinations, non-Hispanic White people made up 69% of those who had gotten at least one shot by April 1, though they account for 60% of the total population. In contrast, Black and Hispanic people accounted for 8.3% and 9.5% of vaccinations, respectively, although they account for more than 13% and 18% of the total population and have experienced higher rates of hospitalization and death from COVID-19. While many have attributed this disparity to vaccine hesitancy and mistrust of the health system, researchers have found that most Americans, irrespective of race, do in fact want a shot. Unfortunately, many people — especially in low-income, minority communities — have an exceedingly hard time finding one.
In our own city of Boston, disparities in vaccination rates are likely attributable, at least in part, to the structure of our vaccination campaigns to date. Massachusetts has arranged mass vaccination sites at sports arenas and convention centers, optimizing for an efficient, high-throughput operation that will safely vaccinate as many people as possible. These sites — like Gillette Stadium, Fenway Park, and Reggie Lewis Center — have been chosen for their capacity and geographic convenience for large swaths of the metropolitan area.
However, the state has not set up mass vaccination sites in some of the communities most disproportionately impacted by COVID-19 in Boston, like East Boston, Chelsea, or Hyde Park. In Chelsea — a city just outside of Boston — only 7% of Latino residents have received vaccines, even though Latino people are 68% of the population. Many individuals in these neighborhoods cannot easily travel to the mass vaccination sites due to disability, work schedules, or lack of transportation. Moreover, obtaining appointments for the mass vaccination sites requires internet access, health literacy, comfort with online registration platforms, and a considerable amount of luck. Indeed, even those who are tech savvy and know the best time to look for appointments online have a difficult time signing up, as appointments are often gone within minutes. The result is a system that consistently leaves behind those who most need a vaccine.
A group of physicians, students, and organizers — including ourselves — noted these structural issues with the vaccine rollout and decided that the vaccination disparities that were evident in the hospitals and communities where we live and work were inequitable but not inevitable.
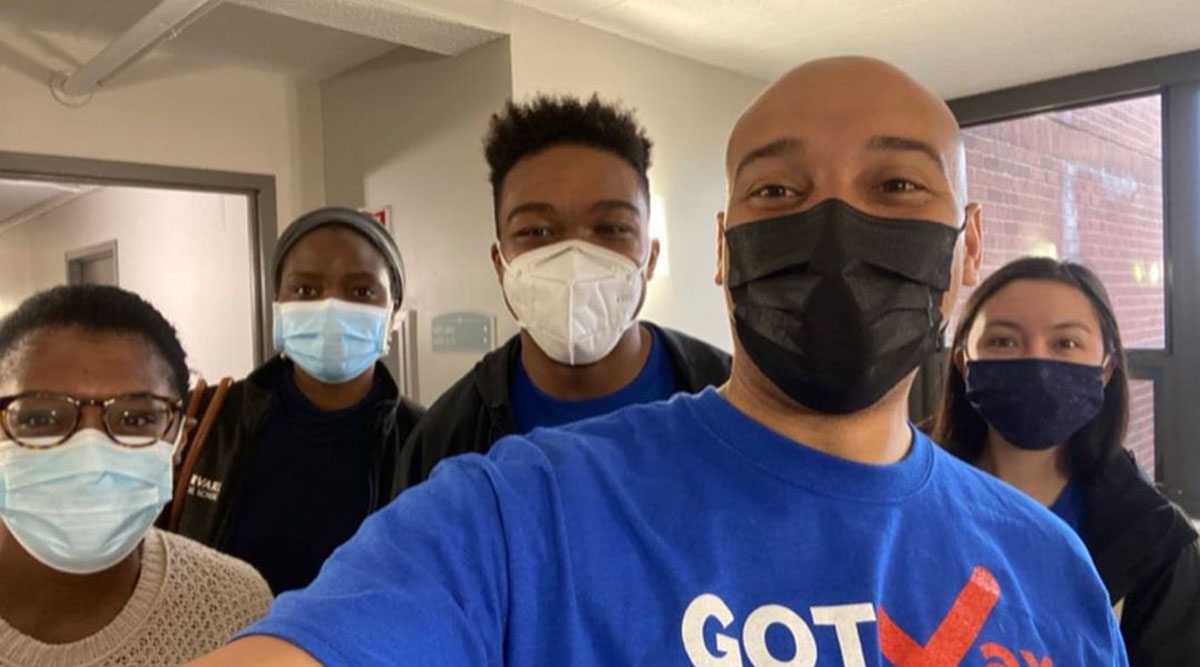
We founded an organization called GOTVax in early March and set out to vaccinate those who have been left behind by bringing the vaccine directly to their doorstep.
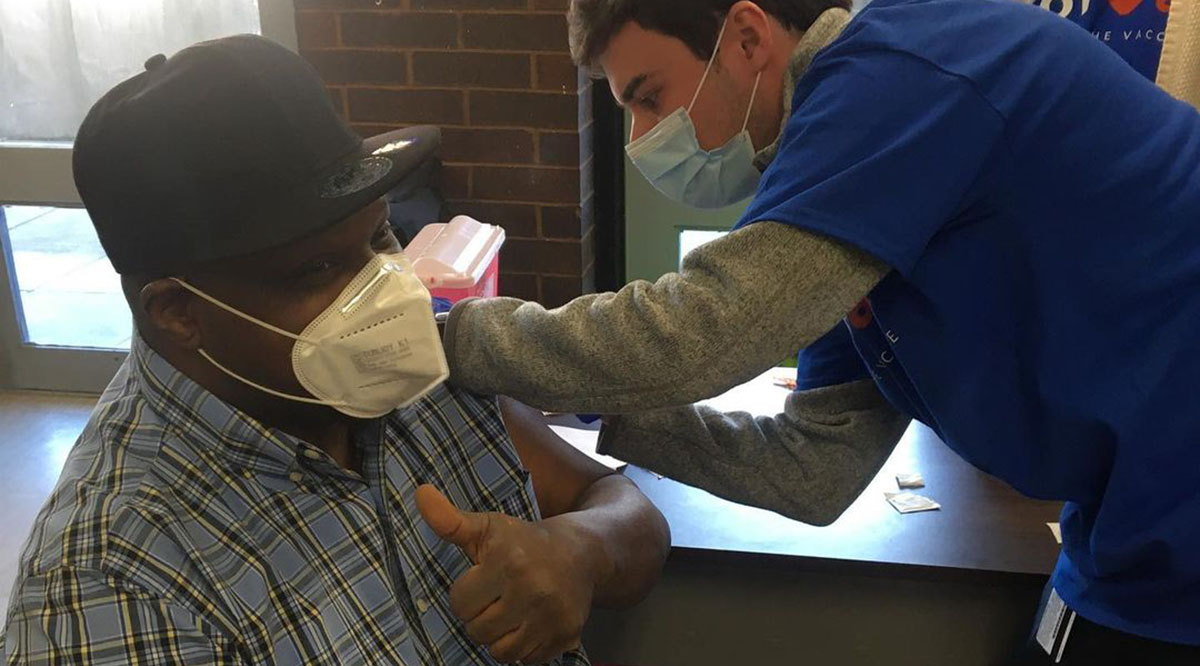
Whereas mass vaccination sites require unvaccinated people to come to them, GOTVax operates on the premise that bringing the vaccine to these communities is an essential strategy as well. In partnership with several local community organizations, including Mascon Medical, the Boston Housing Authority (BHA), and the South End Community Health Center, GOTVax has coordinated pop-up clinics in the lobbies of BHA buildings. These affordable housing units are home to some of the most under-resourced populations in Boston — frequently Black, Hispanic, or Chinese people with an average annual income of $14,000.
GOTVax, true to its name, borrows methods from traditional “get out the vote” campaigns — including phone-banking, text-banking, and door-to-door canvassing — to mobilize individuals in each community where it hosts a pop-up clinic to maximize the number of eligible Bostonians vaccinated. By leveraging physician and medical student volunteers to do this campaign-style outreach, the program has key trusted messengers to communicate with patients about the vaccines.
Over the last month, GOTVax’s coalition of 40 volunteer physicians, students, and community organizers have vaccinated 700 individuals from our most marginalized Boston communities. One community member was a 75-year-old woman who had tried repeatedly to obtain a vaccine at numerous mass vaccination sites to no avail, as appointments were always unavailable. Her story was all too common for her and her neighbors. Nearly half of her building’s residents were unvaccinated despite being eligible and willing for nearly two months. For her, GOTVax “was the best thing because we didn’t have to travel anywhere [and] just came downstairs” to receive the shot.
What have we learned so far?
- Access is still a critical barrier. While we prepared for the possibilities of significant vaccine hesitancy and misinformation — and we have encountered some — we have been surprised by the number of individuals who have been eligible for months but were not yet vaccinated due to difficulty navigating the vaccine sign-up process. These include older adults who meet age-based criteria but lack mobility, those who are unable to navigate complex processes on state websites, and those who do not speak the primary languages offered on vaccine sign-up web portals.
- Grassroots political campaign tactics can be repurposed for vaccine outreach. For many older adults living in poverty, limited access to phones, computers, stable internet access, and other devices makes them challenging to reach. Old-fashioned door-knocking is crucial.
- Community partnerships are key. Our partnership with local community health centers and the BHA allowed us to leverage accurate lists of residents and BHA employees who know and are known to building residents. This allows us to help spread the word about a pop-up clinic, educate about the vaccines, and encourage attendance.
Perhaps our most important lesson learned has been that achieving equity requires more than creating a system that is convenient for many to access. It requires focused investments in efforts specifically dedicated to the populations that are hardest to reach.


