
When doctors at Memorial Health System in Illinois recently got the chance to use an experimental treatment that appears to slow the progress of COVID-19 in some patients — enough to keep them out of the hospital — the decision to move ahead “was a no-brainer,” says Jay Roszhart, president of the Memorial Health System Ambulatory Group.
The ambulatory group has worked throughout the pandemic to lessen the load of COVID-19 patients straining the system’s hospitals, and Roszhart believes preliminary data on the two monoclonal antibodies “pretty clearly showed that with proper patient selection and proper infusion, you would reduce hospital admissions and reduce mortality.”
But not all hospital leaders are so enthused: In places where overextended staff must focus on severely ill COVID-19 patients who jam the wards, some administrators wonder how they can devote caregivers and space to an experimental, laborious treatment for people who might or might not benefit from it. As a result, up to 80% of the more than half a million monoclonal antibody doses that the federal government has shipped to hospitals remain unused, according to Operation Warp Speed, the federal initiative to support COVID-19 treatments and vaccines.
That’s why Francis Collins, MD, PhD, director of the National Institutes of Health (NIH), and Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, met with leaders of AAMC-member medical schools and teaching hospitals on Jan. 15 to urge them to consider using the antibodies more.
“Here is a single kind of therapy for outpatients that does have some evidence, that appears to be safe, and yet it’s being underutilized,” Collins told 200-plus people at the online gathering hosted by the AAMC. Collins supports the therapy, based on preliminary data, as a way to prevent patients from getting sicker and being hospitalized.
Hospitals that are trying the therapy report that their efforts have paid off by reducing admissions for certain patients — but getting there has not been easy.
Promising early results
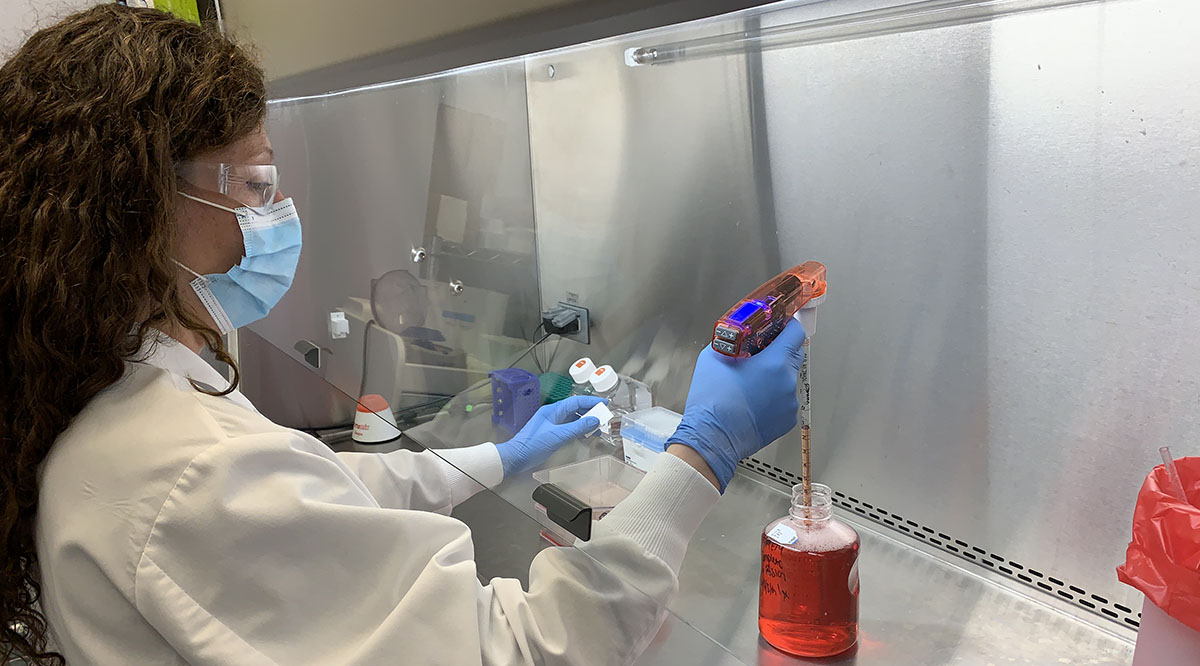
The Food and Drug Administration (FDA) issued emergency use authorizations (EUAs) last November for two monoclonal antibody therapies for COVID-19 — bamlanivimab, by Eli Lilly and Co., and a mix of casirivimab and imdevimab, by Regeneron Pharmaceuticals. Monoclonal antibodies are laboratory-made proteins that, in the words of the FDA, “mimic the immune system’s ability to fight off harmful antigens such as viruses.”
The agency based the EUAs on interim results in Phase 2 clinical trials involving people who had just started showing symptoms and were at risk of getting sick enough to require hospitalization. Among outpatients who got either therapy, 3% were subsequently admitted to hospitals or visited emergency departments, compared with 9% to 10% among those treated with placebos. The randomized, double-blind trials showed similar effects when the results were broken down specifically for patients with various health conditions.
But the EUAs were based on small numbers: 465 patients for the Eli Lilly treatment (including those who got placebos) and 799 for the Regeneron treatment. (Both treatments continue to be evaluated in Phase 2 and Phase 3 trials; Eli Lilly announced more positive results on Tuesday.)
“When you look at the percentages, they’re great,” Fauci said at the recent meeting. “When you look at the numbers, you say maybe not so great.”
Nevertheless, Fauci and Collins said the results have been so consistently positive — and the need to curtail COVID-19 hospitalizations is so severe — that the treatments should be considered more often. Given that the NIH says that the treatments “should not be considered the standard of care for the treatment of patients with COVID-19” but rather should be reserved for certain cases, their request to hospital leaders was gentle.
“Is there a possibility that you might be able to offer this a bit more, on the chance that it might actually turn out to be lifesaving for some people?” Collins asked.
Extra burdens
For many hospitals, the question is not so much about the efficacy of the treatments but rather how much of their scarce resources they should divert to treatments that are still being tested.
The overarching barriers are finding time and space. Administering the antibodies to one person can take three to four hours, says Robert Goldszer, MD, MBA, chief medical officer at Mount Sinai Medical Center in Florida. That includes setting up an infusion station, checking in the patient, administering the infusion for one hour, observing the patient for one hour, checking the patient out of the facility, and cleaning the infusion station to get it ready for the next patient.
The time requirement affects staffing, space, and how many patients can be treated.
Staff
“The first thing we hear from people about the barriers is staff[ing] — every single time,” John Redd, MD, MPH, chief medical officer in the Office of the Assistant Secretary for Preparedness and Response at the Department of Health and Human Services, said at the meeting. “It’s very hard, when hospitals are under such stress” with COVID-19 inpatients, “to get them looking a couple of weeks ahead of time for hospitalizations that will be averted” by antibody treatments.
Hospitals are experimenting with schedule and assignment changes so that nurses and physician assistants can administer the treatments while ensuring that the rest of the hospital remains adequately staffed. In Illinois, Memorial Health System moved some hospital-experienced staff from its primary care and urgent care settings back to the hospital to fill in for staff who are administering the antibodies. Memorial Hermann Medical Group in Texas does the same — and taps into a supplemental staffing pool as well. In Florida, Mount Sinai Medical Center uses existing staff in its emergency department, where the treatments are provided.
Space
Because the patients are positive for COVID-19, they must be treated in areas that are isolated from other patients and staff. In many cases, the therapy is provided in an ambulatory infusion facility where patients with cancer or immunologic disorders receive care as well.
“You have to have a place where patients can be given an IV, treated, and monitored, all for three to four hours,” says Goldszer at Mount Sinai Medical Center. “It’s not easy.”
Mount Sinai Medical Center devoted an overflow wing of its emergency department to the antibody treatments. In Illinois, Memorial Health System uses sections of its ambulatory respiratory care centers, which are off the main hospital grounds. In Tennessee, Vanderbilt University Medical Center walled off part of a former parking garage.
To help safely manage the foot traffic and reduce crowding, hospitals set up appointments in three- or four-hour intervals, such as the 7 a.m. and 1 p.m. slots at infusion centers on the main campus at Memorial Hermann Medical Group in Texas.
But those large blocks of time for each patient severely limit how many can be served. Even though Memorial Health System recently expanded its treatments from six hours a day to 12, the Illinois facility can still treat only 12 patients each day, Roszhart notes.
Patient eligibility
Only certain COVID-19 patients can get the treatments, and the moment a patient gets sick, the clock starts ticking on how long they are eligible.
Patient conditions
The FDA approved the antibodies for people age 55 and above, as well as 12- to 17-year-olds, who do not yet have symptoms that require hospitalization but might be at risk for admission because of conditions that make them susceptible to severe harm from COVID-19. Those conditions include various respiratory ailments, obesity, chronic kidney disease, immunosuppressive disease, and heart disease, and they vary according to age groups.
“You have to have the right patients for this,” Goldszer explains.
Determining the right patients requires several health care workers, often in different locations, guiding a patient through a multistep process that typically involves determining if the patient has mild to moderate symptoms; a positive COVID-19 test; confirming the patient is early in the course of the infection; a referral to be considered for treatment (often provided by a physician who saw the patient); an intake assessment to make sure the person meets the FDA criteria; counseling the patient about the treatment’s potential benefits and risks (the EUAs list the possible side effects as allergic reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting); and scheduling a slot.
“We’re funneling in referrals from across the city,” says Annamaria Macaluso Davidson, MD, MBA, associate vice president of medical operations at Memorial Hermann Medical Group.
Timing of treatment
After getting approved, patients face a tight window to get treatment. The FDA says the treatment must be administered within 10 days of the onset of a person’s symptoms. What’s more, the sooner a patient is treated during the time span, the better the odds of success.
“You want to give this treatment the first week that somebody’s sick,” Davidson explains. “You got to have patients come in quickly” after showing symptoms “and you need that test to be given quickly.”
Hospitals have found ways to accelerate those steps, such as by speeding up the referral and test analysis processes, but sometimes the efforts are still insufficient.
“For a few people approved for the treatment, the disease progressed too quickly” by the time of their appointments to benefit from the antibodies, Davidson says. They were admitted to the hospital.
Results
Hospitals report anecdotal and statistical evidence that the treatments are worth the trouble so far.
“Of those that got it, all of them reported feeling much better,” according to Roszhart at Memorial Health System. “Their symptoms were lessened. They were able to stay in their homes” instead of being admitted to the hospital.
These are among the results reported by a sampling of hospitals, based on recent data:
- Mount Sinai Medical Center, Florida: 440 treated, 19 admitted to the hospital.
- Memorial Health System, Illinois: more than 350 treated, 11 admitted.
- Memorial Hermann Medical Group, Texas: 250 treated, zero admitted.
- UCSF Helen Diller Medical Center, California: 75 treated, one admitted.
As data continue to come in from these front-line experiences and the ongoing trials, Collins acknowledged at the recent meeting, “It is still early for claiming an absolute certainty of benefit.”
For people on the front lines, like Jeanne Noble, MD, at UCSF Helen Diller Medical Center, the benefits have been worth the trouble.
“We look at [bamlanivimab] as an investment in our patients,” says Noble, director of COVID response in the emergency department, where the treatments are given. “It has been really wonderful to have a therapy to offer our COVID patients that may prevent progression to serious illness.”
