Editor’s note 12/12/2023: On Dec. 8, 2023, the U.S. Food and Drug Administration (FDA) announced the approval of CASGEVY, the first FDA-approved therapy that uses CRISPR/Cas9 gene-editing technology. CASGEVY is a treatment for sickle cell disease and was tested in a clinical trial discussed in this article.
It has been more than a year since Markus Mapara, MD, a professor of medicine and director of blood and marrow transplantation at Columbia University Irving Medical Center in New York, first used an experimental CRISPR gene-editing treatment in a patient with sickle cell disease, an inherited blood disorder that can cause severe pain, organ damage, and premature death.
Although the clinical trial is still in early stages and has only been tested in a few patients, so far, the results are promising.
“[The patient is] doing phenomenally well,” says Mapara, who is a hematologist, oncologist, and blood transplant physician. “He has not had a single crisis.”
Sickle cell disease, which currently affects about 100,000 people living in the United States and millions worldwide, is the result of a genetic mutation that produces an abnormal type of hemoglobin, the protein that red blood cells use to deliver oxygen throughout the body. The abnormal cells take on a sickle, or curved, shape, which can clot within narrow blood vessels.
“This is a huge health problem for these patients,” Mapara says. “It has a huge impact on their quality of life and well-being.”
At the moment, a bone marrow transplant from a healthy donor is the only curative option, but this approach can have severe complications.
“You’re running into risks of introducing foreign cells into a recipient,” Mapara says. “[The body] may reject them, or the donor cells might attack the recipient.”
But with the development of CRISPR (which stands for clustered regularly interspaced short palindromic repeats), new opportunities for treatment using the patients’ own cells have opened up.
“[CRISPR is] a tool that scientists and clinicians around the world are using to understand our genetics, the genetics of all living things, and — most importantly — to intervene in genetic disease.”
Jennifer Doudna, PhD, University of California, Berkeley
CRISPR, as it is known today, was developed by two scientists, Jennifer Doudna, PhD, who runs a lab at the University of California, Berkeley, and Emmanuelle Charpentier, PhD, scientific and managing director of the Max Planck Unit for the Science of Pathogens in Berlin, Germany, who were awarded the 2020 Nobel Prize in chemistry for their work on this technology.
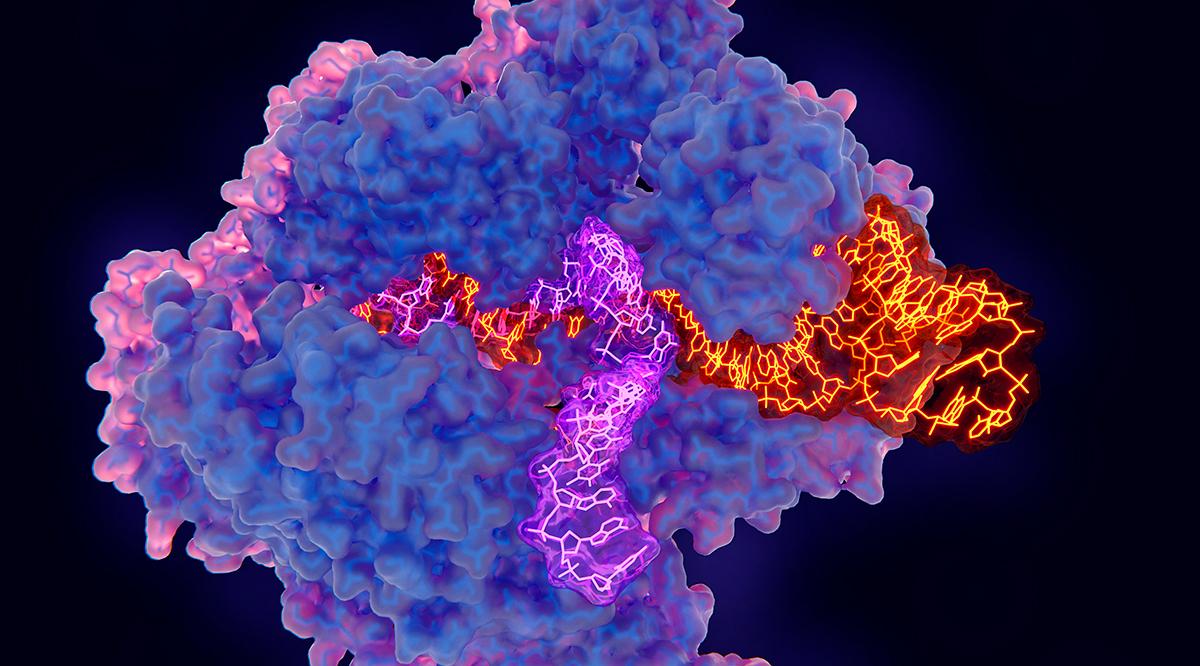
The scientists worked together to uncover precisely how bacteria have evolved to fight off viruses — and to apply that same process to engineer human cells. In particular, Doudna and Charpentier found that an enzyme known as Cas9 can be guided by a programmable RNA to locate specific genetic sequences in any organism. The enzyme then works like a pair of scissors, cutting the DNA’s double helix and allowing for sequences to be deleted, added, or replaced.
“It’s a tool that scientists and clinicians around the world are using to understand our genetics, the genetics of all living things, and — most importantly — to intervene in genetic disease,” Doudna said during a speech at Learn Serve Lead 2021: The Virtual Experience, the AAMC’s annual meeting, in November.
The technology has been celebrated throughout the scientific community as a significant advancement that is changing the way research is done across fields. CRISPR has been used to experiment with gene-edited mosquitos to reduce the spread of malaria, for engineering agriculture to withstand climate change, and in human clinical trials to treat a range of diseases, from cancer to transthyretin amyloidosis, a rare protein disorder that devastates nerves and organs.
Still, the technology comes with significant ethical implications, including ensuring it does not have unintended negative consequences, that it is used equitably, and that a consensus is reached on where to draw the line in the technology’s use.
AAMCNews spoke with researchers, physicians, ethicists, and educators on the cutting edge of CRISPR technology about its enormous potential for both good and harm to the future of humanity.
Potential for good — clinical trials show promise
Sickle cell disease and beta thalassemia
The clinical trial that Mapara enrolled his patient in last year was one of the first to attempt to use CRISPR to treat a genetic disorder in humans.
Though researchers and physicians are pursuing several gene therapy treatments for sickle cell disease and beta thalassemia, a similar blood disorder, this approach targets the gene that stops the production of fetal hemoglobin. Experts have found that people produce fetal hemoglobin up until about three months after birth, at which time their cells begin to produce adult hemoglobin, Mapara explains. It is the adult hemoglobin in people with sickle cell disease and beta thalassemia that takes the irregular shape and causes health problems.
“For a physician-scientist it is a dream come true when you can be part of and witness the development of a revolutionary new treatment modality.”
Markus Mapara, MD, Columbia University Irving Medical Center
“You get rid of the repressor and have enhanced production — again— of fetal hemoglobin,” he says, explaining that the patients who are now producing higher numbers of fetal hemoglobin rather than the mutated adult hemoglobin are experiencing fewer crises.
National Public Radio has been documenting the journey of the first person to join the clinical trial, Victoria Gray, since her first treatment in 2019.
“This is really a life changer for me,” Gray told NPR last December.
Mapara says that the initial results of the clinical trial were published in December 2020 and that follow-up results continue to be very promising.
“This is really a potential game-changer for those patients,” he says. “For a physician-scientist it is a dream come true when you can be part of and witness the development of a revolutionary new treatment modality.”
Leber’s Congenital Amaurosis
CRISPR is also being used in a clinical trial aimed at treating Leber’s Congenital Amaurosis, a genetically determined progressive form of congenital visual loss and blindness.
While there are more than 300 genes that are linked to vision defects, this trial focuses on one gene mutation that causes a particularly severe form of degeneration.
“It’s what we call a problem with splicing of mRNA,” says Mark Pennesi, MD, PhD, who leads Oregon Health & Science University’s involvement in the trial and is the Kenneth C. Swan professor of ophthalmology in the OHSU School of Medicine and chief of the OHSU Casey Eye Institute’s Paul H. Casey Ophthalmic Genetics Division. “The mutation creates a little stop sign in the sequence so the whole protein doesn’t get produced … [for the treatment, guide] RNAs will target sequences on either side of the stop sign, the Cas [CRISPR-associated] protein will cut them out, and the DNA will repair itself. Hopefully, the cells will start to make the protein.”
“It’s groundbreaking. The eye is one of the most accessible parts of the brain and vision is such an important thing for people. This really does open the door for many other therapies.”
Mark Pennesi, MD, PhD, Oregon Health & Science University School of Medicine
Last year, clinicians at OHSU’s Casey Eye Institute performed the CRISPR procedure on a patient, marking the first time CRISPR has been used in a human in vivo, or within the body, as opposed to removing the genetic material for editing.
“It’s groundbreaking,” Pennesi says. “The eye is one of the most accessible parts of the brain and vision is such an important thing for people. This really does open the door for many other therapies … We are hoping we could use CRISPR in neurological or muscular diseases.”
Initial results from the clinical trial involving six patients show that the procedure is safe and that it could improve vision.
“One patient treated at our site has gone public,” he says. “She’s experienced an improvement in visual acuity, she can see objects, and she feels she is actually seeing color.”
Pennesi says they will continue to increase the doses of the treatment in order to monitor if results improve and adds that they hope to eventually make this treatment available to children, who are more likely to experience reduced effects of degeneration.
“It’s really a wonderful time to be in this field because it’s changing from a field where we had no options to now one where we do,” he says.
Cancer
CRISPR is also causing a buzz in the field of cancer treatment.
At the University of Pennsylvania in Philadelphia, physicians and researchers have used CRISPR to genetically engineer immune cells to better fight tumors.
Edward Stadtmauer, MD, section chief of hematological malignancies at Perelman School of Medicine at the University of Pennsylvania and principal investigator of the clinical trial, started working on this project around 2016, when CRISPR technology was very new.
Stadtmauer had long been working with CAR T-cell therapy, which edits the immune T-cells by adding a warhead to the outside that targets cancer cells. While this method has been extremely effective with many blood cancers, Stadtmauer hypothesized that CRISPR could take the treatment to the next level.
Using the technology, Stadtmauer and his team were able to take the patient’s T-cells, remove three genes and add one gene that, together, lengthened the life of the immune cell and made them more potent at targeting cancer. It was the first investigational use of multiple edits with CRISPR to alter the human genome.
“Remarkably, and probably — to me — the most important finding of the study was that these triple gene-edited cells with the additional insertion of another gene actually had tremendous proliferation and expansion ability and continue to survive for nine months to a year later without any sign that they were going down in their number,” Stadtmauer says. He adds that patients who received the edited cells did not experience any serious unintended consequences or severe side effects. “Those things were reassuring and why we consider it to be safe.”
While these results are promising, there is still much research to be done to maximize the technology’s potential in cancer treatment. Blood samples from the three patients involved in the trial showed that the edited cells thrived, but none of the patients responded to the therapy.
“One of the limitations of using your own cells is that the cells may not be as functional in a patient as cells from a healthy, younger person because of age or exposure to chemotherapy,” Stadtmauer says. “And the other problem is that it can take a month or so from the day that the patient gets the cells harvested to actually infusing the cells, and that requires patients who are sick with their disease to have some sort of bridging therapy to keep them well until the product is created. So, the most exciting current approach is to use allogenic or donor immune cells as a source for an off-the-shelf product that can be infused in a timely manner and directed at whatever antigens you want … and there's a tremendous amount of research going on right now in this promising area.”
Advancement with equity in mind
One of the most remarkable things about CRISPR technology is how rapidly it has developed. But as exciting as this is for the advancement of science and medicine, experts in fields ranging from research to bioethics, including Doudna, have cautioned that the advancement should not outpace the tackling of ethical complications that arise.
Among these is determining who will have access to advanced gene therapies.
“We have to really grapple with equity and accessibility,” Doudna said at the AAMC annual meeting. “We have to be cognizant of how to be sure that everyone who can benefit from this technology has access to it.”
This is an issue that Eric Kmiec, PhD, had on the top of his mind in 2015, when he became the founding director of the Gene Editing Institute at ChristianaCare in Newark, Delaware, the only institute of its kind that is based in a community health system.
“All due respect to major medical centers — they do amazing work — but somehow the community cancer center always felt to me to be on the ground in cancer,” Kmiec says. “We ought to think about how those technologies are going to affect all people.”
The Gene Editing Institute has what Kmiec calls a “bench to bedside paradigm.” He and his researchers have offices in the same building where the oncologists are seeing patients. They attend grand rounds and have an open-door policy with the physicians. A surgical oncologist regularly attends lab meetings where research is discussed.
“Interacting with the clinicians almost daily taught me a lot about how challenging this damn thing [treating cancer] is,” Kmiec says. “A lot of really bright people have worked on cancer therapy for years … we have to sculpt our approach on what the clinicians are telling us … usually [researchers] come in and tell clinicians how to use tech. We did the opposite.”

The institute’s commitment to equity goes beyond the development of therapies that reach underserved populations; it also extends to diversifying the recruitment base for the next generation of CRISPR scientists. In a partnership with Delaware Technical Community College, it created CRISPR in a Box™, an educational kit that gives high school and community college students the tools to study and use CRISPR in the classroom. The resource has been accompanied by a concerted outreach effort that includes instructional videos and opportunities for students to interact with scientists through Zoom to help explain the technology.
Kmiec is hopeful that lighting the spark of interest in CRISPR and showing young people, particularly people of color and those who come from under-resourced communities, that using this technology does not require an advanced degree will inspire a more diverse labor force in the future.
“We want to engage communities of color not just to learn about something we already know about, but to engage directly in [its development],” Kmiec says. “[That way] the minority groups will be standing with us at the finish line.”
CRISPR and ethics — where do we draw the line?
Austin Keeler, PhD, a postdoctoral student at the University of Virginia, uses CRISPR in the lab to alter the genetic makeup of mouse embryos to create transgenic animals for research. Though he finds CRISPR’s potential exciting, he thinks a lot about its ethical implications on issues that currently resemble science fiction more than reality. These thoughts inspired the subject of a course he teaches to undergraduate students entitled “Homo CRISPR — Future Humans?”
Keeler provides his students with resources to explain how gene editing works and then opens up classroom time to discussions about a variety of its current and potential uses: from gene-editing mosquitoes to control the spread of malaria to the use of CRISPR for cosmetic changes in humans.
“I wanted to hammer home how fast we’ve moved into this technology and how much potential it has to drastically change our lives,” Keeler says. “It is going to have profound ramifications in their adulthood and in the lives of their children. I’m not sure how much of what is happening has made its way to outside of academia.”
These ethical issues have made headlines in recent years. In 2018, a Chinese biophysicist, He Jiankui, announced to the world that he had created the first genetically altered babies. He had used CRISPR to edit the germline of three embryos to make them less susceptible to HIV.
The announcement was met with outrage from scientists and ethicists alike and He was ultimately sentenced by the Chinese government to three years in prison for illegal medical practice. It was a reminder that the technology, which is so efficient and easy to use, has the potential to be abused without clear regulations and oversight.
“Like any new technology, CRISPR comes with risks,” Doudna said at the AAMC’s annual meeting. “It was clear early on that there were going to be some real ethical challenges.”
In an effort to facilitate public discourse on these challenges, Doudna will be participating in the Third International Summit on Human Genome Editing in March 2022, where stakeholders from across the world will discuss the current state of the science as well as ethical and cultural considerations, the development of regulations, and the role of the public in directing the research agenda, among other issues.
Christopher Scott, PhD, a bioethicist and the Dalton Tomlin professor of medical ethics and health policy at Baylor College of Medicine in Houston, Texas, is currently working on a National Institutes of Health-funded project that will be the first comprehensive empirical study into how society might go about regulating the ethical use of genome editing moving forward.
“Like any new technology, CRISPR comes with risks … It was clear early on that there were going to be some real ethical challenges.”
Jennifer Doudna, PhD, University of California, Berkeley
Scott’s team has met with dozens of people, including lawyers, disability rights advocates, ethicists, and futurists, but has also focused on engaging members of the public who are not regularly involved in discussions about scientific technology.
“We get their feedback about their opinions and values,” Scott says of the members of the public. “The results have been super eye-opening.”
As part of the study, groups of laypeople were presented with different future scenarios involving gene editing and were asked about their comfort level with them. Scott has found that, in general, there is a major distinction between somatic cell editing, which is the altering of often disease-causing genes that are not involved in reproduction, and germline editing, which changes heritable traits.
“With germline editing, the answer was, generally, ‘We shouldn’t do that yet,’” Scott says. “One question [posed] was, ‘If it were as safe as we could make it, [should it be done?] … There were not a lot of unanimous, absolutely, yes we should do that [answers].”
Keeler observed similar reservations among the students in his class. Many of the students were disturbed at the idea that a human’s genetic traits could be changed without their consent. Some worried that, if someday it is possible to enhance certain traits that are perceived as beneficial, it might further increase inequities between the “super” elites and people not afforded such enhancements.
“You have all the normal ethical issues that arise in the context of using technologies that can be used in ways one might find problematic,” says Inmaculada de Melo-Martin, PhD, a professor of medical ethics in medicine at Weill Cornell Medicine Medical College in New York. “[For example,] selecting for particular traits, or against particular traits, [and] what this means for the things we value.”
Although some of these technologies are not yet possible, Scott says that it’s important to create clear governance structures and ethical guidelines now before the next generation of gene editing technologies develop.
“There is a way to deliberate this with foresight rather than with hindsight,” Scott says.
So far, there is little international consensus on what is acceptable when it comes to experimental gene editing in humans. In the meantime, responsibility rests on researchers and the institutions that support them to examine the ethics of their own work.
“This technology is so powerful. It can provide so many benefits it’s easy to just put aside the possible concerns and say we will solve those problems when they arise,” de Melo-Martin says. “My concern is that the possibilities, the promises of these interventions, are so significant that it can prevent us from realizing we need to be careful and pay attention to what the consequences might be.”