Universities are often known for silos, but on many campuses, COVID-19 is creating something indispensable for fighting the pandemic: collaboration. In response to widely reported shortages of personal protective equipment (PPE), testing swabs, hand sanitizer, and other supplies, medical schools nationwide are working with colleagues in engineering and other departments to design and produce these necessities.
Here’s an inside look at four success stories that involve harried production schedules, supply chain issues, exhaustion, exhilaration, and partnerships that might never have occurred otherwise.
The University of Virginia
On March 18, William Guilford, PhD, received an email request from an intensive care nurse at UVA Health. Could the University of Virginia School of Engineering and Applied Science produce PPE — from N95 masks to face shields — using 3D printing?
“I always tend to put on my engineer hat first, and I wasn’t sure that creating an N95 mask was a realistic goal,” says Guilford, assistant dean for undergraduate education and associate professor of biomedical engineering. “But my nonengineer hat was just, ‘Whatever you need, you tell us, and we’ll make this happen.’”
Guilford soon hosted a Zoom meeting with colleagues ranging from professors in the biomedical engineering department to an executive MBA student who works at Thomson Reuters (a business information services company) and helped build a materials sourcing and product distribution network. Engineers worked with UVA Health to establish equipment priorities, including cotton masks, face shields, and nasopharyngeal swabs for testing. They quickly discovered that the biggest obstacle — one faced by organizations across the country — was shortages of raw materials, from clear plastic to elastic. “It’s hard stuff to find now,” says Guilford. “In a previous world, you would buy elastic at the local fabric store.”
“I always tend to put on my engineer hat first, and I wasn’t sure that creating an N95 mask was a realistic goal. But my nonengineer hat was just, ‘Whatever you need, you tell us, and we’ll make this happen.’”
William Guilford, PhD
University of Virginia School of Engineering and Applied Science
Despite the competition for materials, the UVA team obtained enough to begin production, and Guilford ensured that the process included an engineering design approach: “Everything needs to be tested and iterated,” he says. The teams have produced not only masks but also ear protectors (mask straps that hook around the back of your head rather than digging into your ears, which was a problem for intensive care unit nurses working 12-hour shifts) — and they’re now working on face shields and swabs.
“We’re doing something that universities don’t tend to do: We’re in some sense manufacturing, and we’re trying to hit a scale where we can meet our needs and the needs of the surrounding community for the long term,” he says. “We’re doing that for face masks. We’re working on that for swabs and getting very close.”
The grassroots effort is now producing thousands of face shields along with hundreds of masks for UVA Health and local hospitals. Engineers are even developing an N95-like mask, but it’s challenging, and it takes about 10-14 hours to print the prototypes.
“The N95 standard is stringent for filtering capability, which is just one part of it, but the other part is that a ton of engineering went into designing a mask that is deformable and sits tight enough to the face that it completely seals it,” he says. “Because if all air has to do is go around, say, your nose or around your chin or cheek, it doesn’t matter how good the filter is. You’re not filtering it anymore. So we got a reality check very quickly on this.” (UVA Health also is using a robot to disinfect up to 6,000 N95 masks per day.)
As the effort develops, more than 60 people are involved, including not only UVA faculty but also local citizens and business leaders. “I consider myself blessed,” Guilford says. “I think everyone who is involved in this would say they feel tired but lucky. We get to help. Every day brings just a frightening urgency.” And despite the pressures, he still thinks like an engineer. “When I feel like this needs to be done tomorrow,” he says, “I remind myself that it needs to be done right.”
Ohio State University
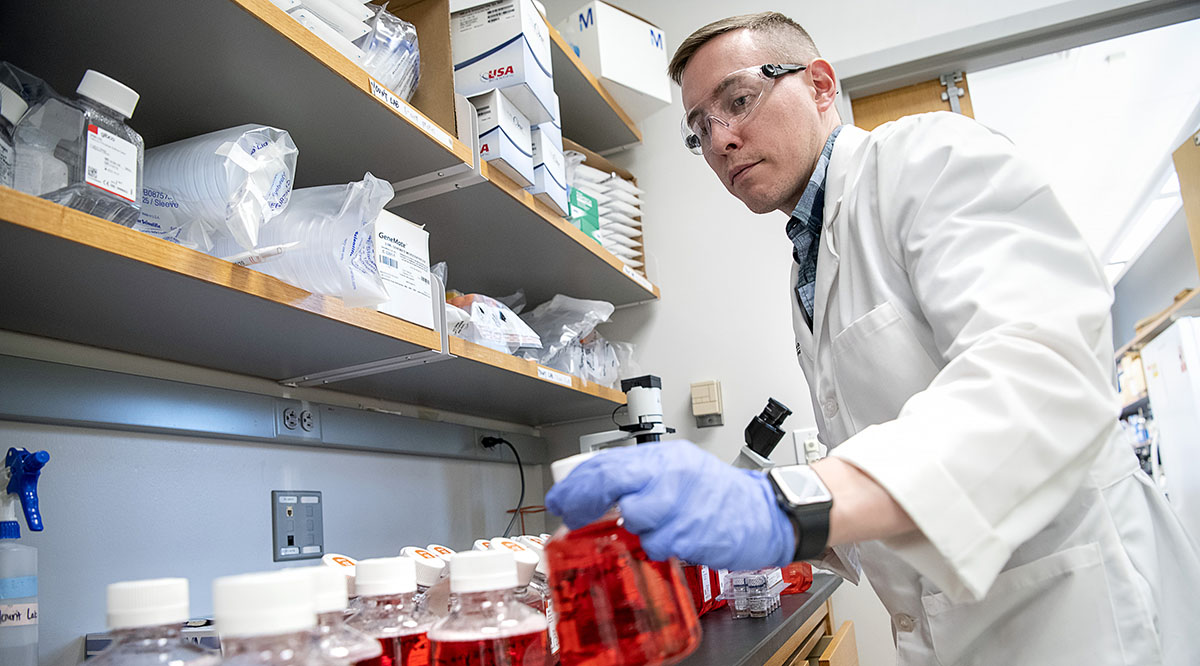
Before the pandemic, no one really discussed viral transport media (VTM), a salt solution that stabilizes pathogens for testing. But in mid-March, the Ohio State University Wexner Medical Center was facing a VTM crisis.
“It was dire — if we didn’t have this media the next day, we were going to have to stop testing,” says Peter Mohler, PhD, vice dean for research at the Ohio State University College of Medicine and director of the Dorothy M. Davis Heart and Lung Research Institute. Mohler called some Ohio State immunologists and microbiologists about producing VTM, and within hours, the group had reviewed Centers for Disease Control and Prevention and World Health Organization (WHO) guidelines and gathered raw materials from on-campus supplies.
“They worked all night and by the next morning they’d come up with not only a solution, but they’d started to produce sterile viral transport media,” says Mohler. “Obviously, we needed to work through our pathology labs to do quality control and testing on it, but sure enough, it worked. And quickly we were up and running.”
Each test kit uses about 3 milliliters of VTM, and by mid-April, Ohio State had created enough VTM for up to 30,000 kits (it continues to use commercially produced VTM when available). The university has also addressed shortages of nasal pharyngeal swabs in an effort involving a variety of groups, including the Institute for Materials Research, the Center for Design and Manufacturing Excellence, and the Infectious Diseases Institute.
“I hope that when we get out of this, that those sorts of relationships continue, because we can move so much more quickly. … It’s critical that we design our research infrastructure to deal with real-world problems. We can never forget that we're here to make a difference in people's lives.”
Peter Mohler, PhD
Ohio State University College of Medicine
“I’ve never seen anything quite as amazing as this from a collaboration standpoint,” says Jay Sayre, PhD, director of innovation for the Institute for Materials Research. “This goes across our state government, the College of Medicine, our Wexner Medical Center, our Office of Research, our College of Engineering, and manufacturers in Ohio. Even our College of Dentistry has been involved in helping us in the last few steps of the manufacturing process by doing packaging and sterilization for us. You can’t help but be proud of the whole state of Ohio for how everyone has come together.”
On April 17, the first several thousand swabs arrived at Ohio State. The goal is to produce “well over 100,000,” says Sayre. The Wexner Medical Center has also worked with Battelle, which conducts research and designs and manufactures products, to develop a COVID-19 test that offers a faster turnaround time on test results. And Ohio State engineers collaborated with the College of Medicine to produce protective shields.
“Like most academic medical centers, a lot of our work was in silos, whether that was the research silo, or the clinical mission silo, or the education silo,” says Mohler. Since the crisis began, however, senior leadership teams from across campus have met daily. “I hope that when we get out of this, that those sorts of relationships continue, because we can move so much more quickly,” he says. Mohler also hopes the pandemic will inspire leaders to rethink research priorities. “It’s great to publish papers and be keynote speakers,” he says, “but it’s critical that we design our research infrastructure to deal with real-world problems. We can never forget that we're here to make a difference in people's lives.”
The University of Massachusetts
When six students in the Graduate School of Biomedical Sciences at the University of Massachusetts (UMass) Medical School realized that hospitals were desperate for sanitizer, not simply to clean hands but also to sanitize PPE, they quickly took action. In less than three days, they produced nearly 130 gallons of sanitizer.
How did it happen? After researching WHO and Food and Drug Administration guidelines, the students submitted a proposal, which was approved five days later by the UMass Medical School administration. The team also worked closely with the university’s Environmental Health and Safety department and Environmental Building Services department to ensure they complied with the campus’s safety guidelines. Speed would be essential. “On the sixth [of April] they said, ‘We need you to get this done by the eighth because we’re expecting a surge this week,” says one of the students, Tomás Rodríguez, an MD-PhD candidate.
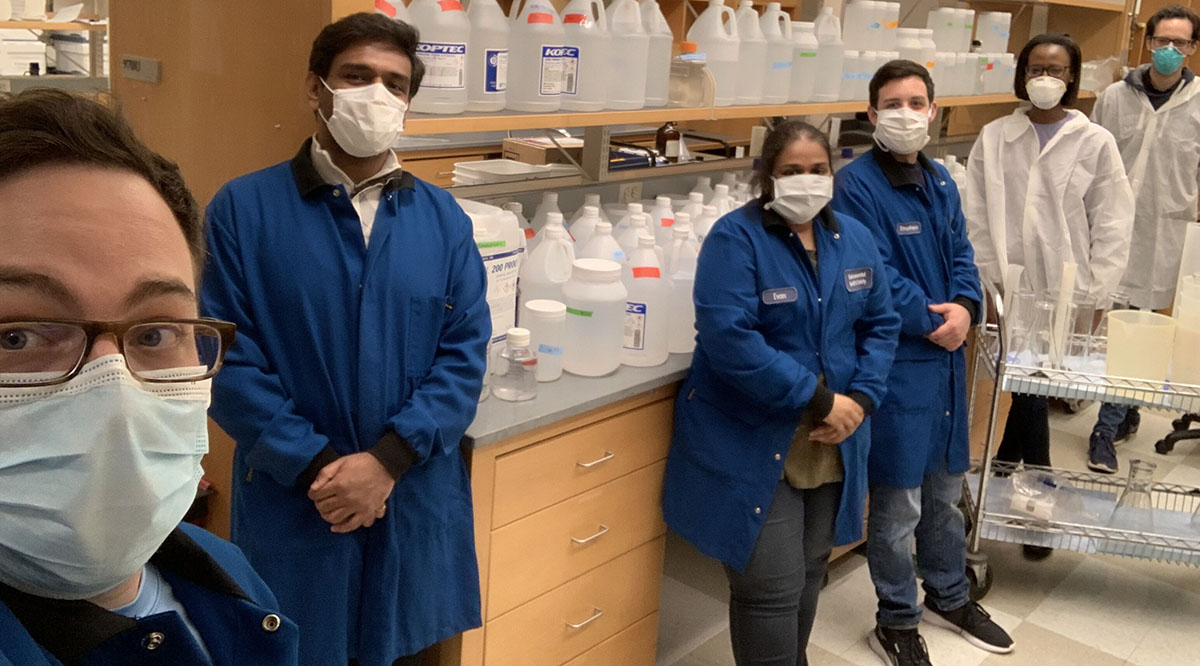
The sanitizer recipe required four ingredients: Hydrogen peroxide, ethanol, glycerol, and water. “We realized that a lot of different biomedical labs across the campus had the necessary ingredients,” says Peter Cruz-Gordillo, an MD-PhD candidate and a UMass Medical School Student Trustee. Various deans sent wide-ranging email alerts, and in 16 hours, the students had received 120 gallons of ethanol. A professor of biochemistry and molecular pharmacology also provided hydrogen peroxide.
The students were temporarily deemed essential personnel, which allowed them to work on campus. To protect themselves from COVID-19 exposure, they wore lab coats, gloves, gowns, and masks, and they also worked in different laboratories.
The students’ sanitizer is high-grade. Most commercial hand sanitizers are about 60% ethanol and don’t necessarily contain hydrogen peroxide. The UMass sanitizer is 80% ethanol, and to prevent allergic reactions, it contains no perfumes or oils. Because of the tight schedule, students didn't have time to order containers, so they sanitized the ethanol bottles and filled them with the sanitizer.
The sanitizer is being used not only at the UMass Memorial Medical Center but also at a local field hospital where Cruz-Gordillo works as a volunteer. A student-led COVID-19 volunteer task force is also overseeing more than 25 different projects, including collecting PPE for hospital use from sources such as on-campus labs and local companies (so far, students have obtained about 20,000 pairs of gloves and 1,400 N95 masks). For Cruz-Gordillo, the experience has been both rewarding and inspiring. “It made me extraordinarily happy and proud to be in a school and a community and a health care system that inspires students to get involved and then supports them in their endeavors,” he says. “It has given me a lot of hope and excitement about going into this field.”
Georgia Tech and Emory University
Susan Margulies, PhD, is uniquely qualified to work with clinicians and engineers during the COVID-19 crisis. She’s a biomedical engineer with a background in mechanical engineering and her research areas include ventilator-associated lung injuries. But what’s really unique is this: Margulies is chair of the Wallace H. Coulter Department of Biomedical Engineering, which belongs to both Georgia Institute of Technology and Emory University. So when Margulies attends leadership meetings at Emory, and hears the challenges faced by Emory Healthcare, she also knows how Georgia Tech can assist (and who she could contact).
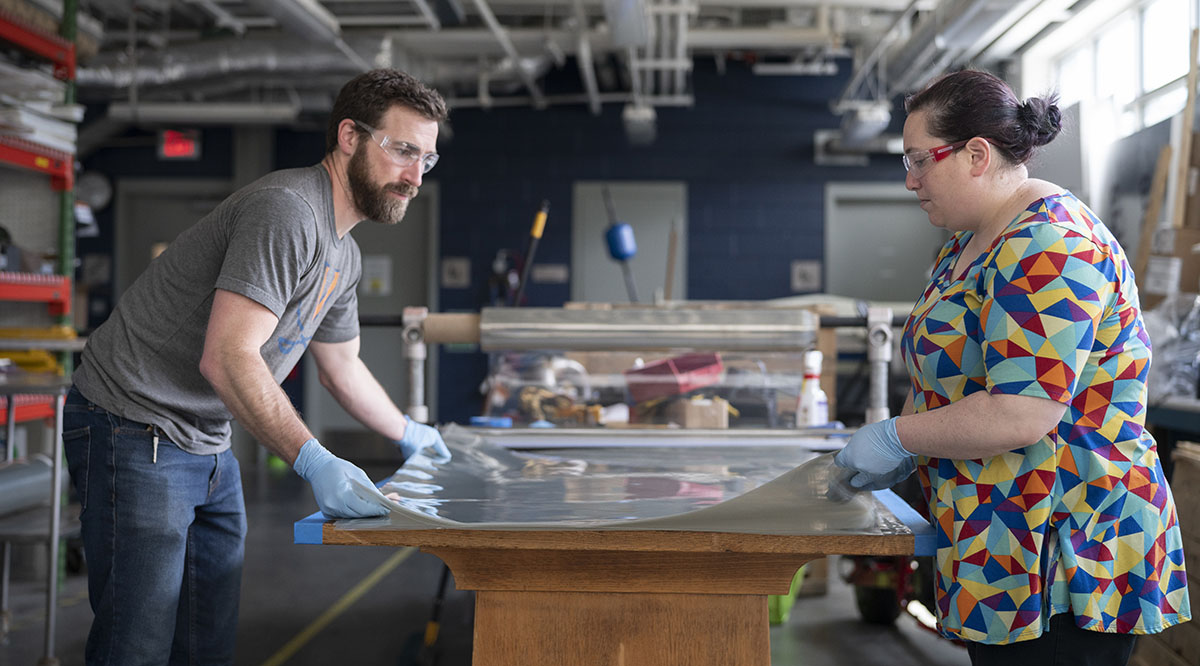
That unusual structure is providing a cross-disciplinary approach to equipment problems during the pandemic. Take face shields, for example. Once Emory Healthcare identified this as a need, Georgia Tech engineers consulted with Emory’s infection prevention experts and nurses, developed several designs, and produced prototypes at the institution’s Invention Studio, a student-run space for building just about anything (including robots). Emory nurses tested the prototype — as did workers at four other health systems — and offered feedback.
“It is so special for clinicians to interact with entities that don't just fulfill your orders, they actually work with you to design the right answers to your questions,” says Margulies. “I think clinicians are truly enjoying this engagement.” And the collaboration between clinicians and engineers, she believes, will continue long after the current crisis. “In biomedical engineering, over 95% of the undergraduate capstone projects are initiated by clinician ideas,” she says. “I think there will be more clinician ideas. And those students who will be working on the projects will spill out into other majors beyond biomedical engineering.”
“We're working on novel ventilators, we're working on special protection for intubation and excavation, we're working on innovative ways to sanitize and reuse materials. … This is a great time to be a biomedical engineer.”
Susan Margulies, PhD
Georgia Institute of Technology and Emory University
Once clinicians provided input on the face shields, engineers settled on two final designs: One features a reusable frame and disposable shields, while the other can be sanitized and reused. Georgia Tech engineers are now working with outside manufacturers to produce thousands of shields a day (and companies such as Georgia Pacific have donated materials).
“We’re not set up to do high-volume manufacturing,” says Kentez Craig, the Invention Studio’s shop manager and a grad student in mechanical engineering at Georgia Tech. “We’ve been focused on handing off the prototype to a mass manufacturer and telling them do this, do this, do this. And then we’ll be able to help a lot of people.”
The efforts go well beyond PPE. “We're working on novel ventilators, we're working on special protection for intubation and excavation, we're working on innovative ways to sanitize and reuse materials,” says Margulies. And the goal is to provide equipment throughout the state: Emory and Georgia Tech have already provided shields to the Georgia Emergency Management and Homeland Security Agency and the Federal Emergency Management Agency.
“There’s intense satisfaction in working on something that is an urgent and important problem,” says Margulies. “This is a great time to be a biomedical engineer.”