Jack and Hank* are best friends, and both are members of the “BMW” club, or Black Men Walking. Every Saturday morning, they meet as part of this informal group, and they not only walk, they talk. They talk a lot, almost nonstop. What do they talk about? Hank is going through some serious marital problems and Jack is feeling the stress of paying for two college tuitions, a mortgage, a car loan, entertainment, and more. None of this comes up. Also, neither has said so, but they both have high blood pressure and are borderline diabetics, and one of them suffers from symptoms of depression and anxiety.
How could they not know all this about each other?
When one asks the other “what’s goin’ on,” the other always responds, “great,” “fantastic,” or “I’m good,” and then they move on to their favorite topics: sports, cars, TVs, work, more sports, larger TVs, and other “safe” subjects. Jack and Hank do not talk about what’s really “goin’ on” with them. Rarely do they talk about their health. They practically never talk about feelings or about sources of their insecurities.
Jack and Hank suffer from “Tough Guy Syndrome” (TGS).
There are serious downsides to being a “tough guy,” and “manning up” can lead to a man going down.
The Man Up Man Down Research Program, a Michigan-based initiative that explores the physical and emotional health of African American men, learned about TGS through 25 focus groups in six cities between 2010 and 2018(Neighbors, 2018; Key, Hayman & Neighbors, 2018). Everywhere, we asked participants what it means to be a “real man.” Although certainly there is no one way to be a man, we found the phrase was a good way to begin discussing notions of manhood. Our research showed that many African American men think being a “real man” means providing for family, achieving the respect of others, and attaining financial success. We also found that it often means being tough and self-sufficient, and that many African American men embrace TGS as a source of self-esteem and self-respect. This may particularly be the case when African American men feel they’ve been given a terribly raw deal in terms of quality education, socioeconomic opportunities, and racial discrimination.
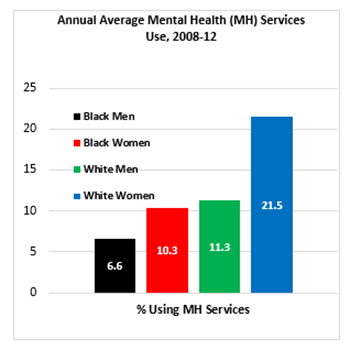 Source: Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2008-2012 (2008-2010 Data – Revised March 2012).
Source: Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2008-2012 (2008-2010 Data – Revised March 2012).
But there are serious downsides to being a “tough guy,” and “manning up” can lead to a man going down.
Although major depressive disorder (MDD) is less common among African American men than white men, African American men with depressive symptoms often are misdiagnosed. What’s more, African American men face more chronic MDD and greater impairment from it. For example, African American men more often experience severe effects in their work life — 37.2% compared to 28.9% among whites — as well as in their relationships. And when African American men experience serious mental health challenges, they far too infrequently get the help they need; in fact, non-Hispanic African American men seek mental health services significantly less often than whites and African American women.
Much too often, we African American men advise each other to “man up” to personal problems. “Handle your business,” we say. This communicates two unhealthy messages. First, it says, “I cannot help you.” Second, it recommends using individual problem-solving strategies without seeking the help of others. Of course, sometimes significant time alone spent praying, meditating, and strategizing is helpful. But TGS forces men to engage in “manning up” to such an extreme that they cut themselves off from family, friends, and professional help — and even from themselves.
We must stop telling each other to “man up.” And we must start telling the truth about how we really feel. African American men and women also must help shift a culture that sometimes frowns upon professional help-seeking. And researchers and members of the medical community must contribute as well through research exploring the many barriers to help-seeking among African American men.
We must stop telling each other to “man up.” And we must start telling the truth about how we really feel.
Obviously, pressure to display a “tough guy” image is not the only reason that African American men are reluctant to seek mental health care. Another factor is a general mistrust of the medical system as well as mistrust of mental health providers. In addition, many African American men are not sure how to seek mental health services — yet at the same time they do know that it can be expensive. Another barrier is an overemphasis on psychiatry as the main source of mental health treatment, which worsens worry about the use of antidepressants, a form of treatment that many African American men dislike. What’s more, African American men may not feel comfortable talking about personal matters with someone they feel is quite different culturally or socioeconomically.
We need to deal with all of these obstacles. The costs of suffering are too great, and there are many benefits to seeking professional help. I know this from personal experience.

My story is both simple and complicated. Years ago, after the unexpected loss of an adult child, I literally had trouble getting out of bed and barely had the energy to shower. Back then, what kept me going was my own personal walking club. I asked my closest friends to join me for a walk once each week, and they readily agreed. My friends gradually helped walk me back to health. And I tried to open up more about how I was feeling to people in general.
In addition, I sought out individual psychological counseling. I remember feeling both anxious and hopeful when my therapist told me that, together, we needed to go into the “heart of the darkness.” But having someone to whom I could talk about my deepest secrets and fears ultimately was even more helpful than the walking group.
Today, I still don’t always share everything that is going on with me. I still sometimes live my life behind a mask of invincibility. It is very comfortable, and it has gotten me through some tough times. But I also try my best to be “real” because doing so helps others and it makes me feel good inside.
I wish that same feeling for African American men — for all men.
Unfortunately, men of all colors have learned to quickly convert hurt feelings to anger. But we only think we are mad. Rather, we are hurt, and TGS won’t allow us to admit it. I say, let’s admit it and then find the origin of that pain. Let’s go directly toward the source of our insecurities and work on them.
So where do we go from here?
First, men need more programs focused explicitly on open, honest dialogue about stress, feelings, and emotional well-being. This is the next step for the Man Up Man Down program. Although the Man Up Man Down program was created as a research project and not a counseling intervention, the vast majority of men who participate say the mere act of meeting and talking makes them feel better. Another next step is to conduct research evaluating more rigorously whether these kinds of discussion groups can mitigate feelings of anxiety and depressive symptoms.
I remember feeling both anxious and hopeful when my therapist told me that, together, we needed to go into the “heart of the darkness.”
We also need to help reduce stigma around help-seeking in African American communities by working with institutions like churches and barbershops. For example, Stephen Thomas, PhD, created the Health Advocates In-Reach and Research (HAIR) program, which is building a national network of barbershops and salons that partner with a university and hospital to address local health needs. In addition, we need to encourage more African American men to become mental health providers. Finally, we need to continue to train mental health providers to be attuned to the culturally unique needs of African American men, which include different vocabularies of distress, the intergenerational impact of slavery, and present-day racial discrimination.
If I could pick one place to start, though, I would ask African American men to talk to someone, just one man, about what’s really goin’ on. “If you feel something, say something.” And I say to all men, try not to catch your death of TGS. Be a Healthy Man, not a Tough Guy.
*Not their real names.
Harold “Woody” Neighbors, PhD, is a C.S. Mott Endowed Professor of Public Health and Family Medicine at the Michigan State University College of Human Medicine and Director of the Man Up Man Down men’s health program. He is also Professor Emeritus of Public Health at the University of Michigan School of Public Health and Research Emeritus Professor in the Program for Research on Black Americans and the Resource Center for Minority Data, Institute for Social Research at the University of Michigan in Ann Arbor, Michigan.